With increasing gestational age, the risk of
MSAF rises and peaks in post-term pregnancies at 30%. Regardless of foetal age,
elevated MSAF incidence is seen in the presence of feto-maternal stresses like
hypoxia and infection [3]. Meconium transit is a common postnatal
event; in the first 24 to 48 hours following birth, about 98% of healthy babies
pass meconium [4]. Foetuses that are 37 weeks or older are the
source of more than 98% of MSAF cases [5]. MSAF is generally
infrequent in preterm deliveries and is more frequently linked to post-term
pregnancies [5,6].
MAS management is a major difficulty for
neonatologists. It is advantageous to employ tactics like improving intrapartum
surveillance and preventing post-term pregnancies. The use of positive
end-expiratory pressure, surfactant therapy, high-frequency oscillatory
ventilation, and inhaled nitric oxide, among other recent developments in the
understanding and management of acute lung injury, have significantly improved
the results of mechanical assisted breathing (MAS).
The objective of the present study was to
evaluate the clinical features of meconium aspiration syndrome (MAS) in
newborns, with particular attention to birth weight, gestational age, and the
immediate consequences of these findings.
MATERIALS AND METHODS- This prospective study was conducted at SVP PG
Institute of Pediatrics, affiliated with SCB Medical College and Hospital,
Cuttack, over one year (November 2020 to October 2021). Out of 5460 newborn
admissions during this period, 4892 newborns exhibited respiratory distress,
with 780 having a history of meconium-stained amniotic fluid (MSAF). The study
focused on 96 cases (out of 780) of meconium aspiration syndrome, approved by
the Institute's ethical committee.
Diagnostic Criteria for Meconium Aspiration
Syndrome:
1. Presence of meconium-stained amniotic fluid.
2. Tachypnea, retractions, grunting, or other
abnormal signs on physical examination consistent with pulmonary disease (onset
of respiratory distress within 24 hours of life).
3. Need for supplemental oxygen or ventilator
support.
4. A chest radiograph consistent with aspiration
pneumonitis.
Study Population- The study included 96 newborns with meconium staining and who developed
meconium aspiration syndrome, forming a heterogeneous population. Cases were
selected from the general newborn wards and neonatal intensive care unit,
including the ICU step-down ward, at SVP PG Institute of Pediatrics, and were
followed up for their immediate outcomes.
Selection of Cases and Methods- All preterm, term, and post-term infants, delivered by various means,
meeting the criteria for MAS, were included through purposive sampling.
Exclusion criteria encompassed newborns with other respiratory conditions,
congenital issues, sepsis, and those without respiratory distress despite
meconium-stained amniotic fluid.
Data Collection- A detailed antenatal and natal history was obtained to identify the
etiology of meconium passage. Postnatal history included Apgar score, birth
asphyxia, and complications, with details of resuscitative measures.
Gestational age assessment utilized Ballard's score. Routine investigations and
radiological assessments were conducted, with management tailored to the
severity of respiratory distress.
Statistical Analysis- Data entered in MS-Excel 2019 underwent correction for typographical
errors and analysis using SPSS 16.0. Chi-square tests compared qualitative
data, with a significance level set at 95% (p<0.05).
RESULTS- In our study, prolonged labor was found to be
the most common (n=25, 26%) factor associated with MAS followed by
Pre-Eclampsia (n=22, 22.9%), Anemia (n=19, 19.8%) and oligohydramnios
(n=12,112.5%).
Table 1: Maternal Risk factors associated with MAS
|
Maternal Risk Factors |
No. of cases |
Percentage |
|
Anemia |
19 |
19.8 |
|
APH |
7 |
7.3 |
|
Cord around neck |
1 |
1.0 |
|
Oligohydramnios |
12 |
12.5 |
|
Preeclampsia |
22 |
22.9 |
|
Prolonged Labor |
25 |
26.0 |
|
PROM |
10 |
10.4 |
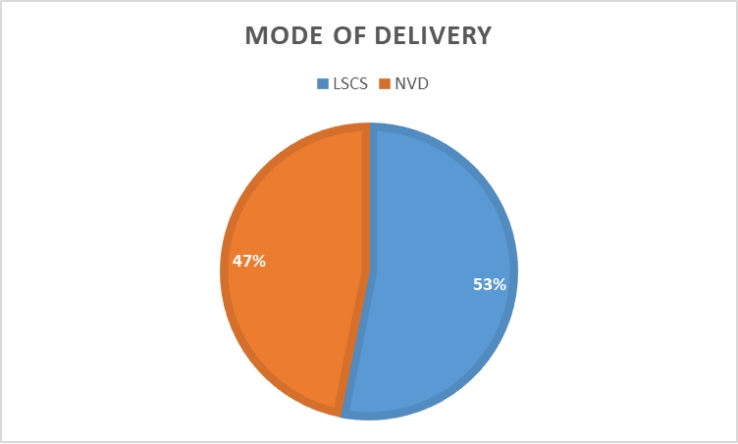
Fig. 1: Mode of Delivery and MAS
In our study, babies
with MAS born by normal and assisted vaginal delivery formed 46.9% of cases and
babies born by Caesarean delivery 53.1%.
Table 2: Gestational age and MAS
|
Gestational Age |
No Cases of MAS |
Percentage |
|
<34 weeks |
3 |
3.1 |
|
34-36 weeks |
5 |
5.2 |
|
36-38 weeks |
15 |
15.6 |
|
38-40 weeks |
62 |
64.5 |
|
40-42 weeks |
11 |
11.4 |
In the present study, most
of the cases of MAS occurred in term babies with a mean gestational age of
38-40 weeks. 62 (64.5%) babies belonged to 38-40 weeks of gestation and
11(11.4%) babies were of 40-42 weeks of gestation. 2 (6.89%). MAS was also seen
in preterm babies. 5 (5.2%) cases were of 34-36 weeks of gestation and 15
(15.6%) belonged to 36-38 weeks of gestation. 3 cases (3.1%) were born before
34 weeks of gestation.
Table 3: Birth weight and MAS
|
Birth Weight |
No of Cases of MAS |
Percentage |
|
1.5-1.9 kg |
12 |
12.5 |
|
2-2.4 kg |
26 |
27.0 |
|
2.5-2.9 kg |
36 |
37.5 |
|
3-3.4 kg |
16 |
16.6 |
|
3.5-3.9 kg |
6 |
6.2 |
The mean birth weight of
babies with MAS was 2.55 kg (1.0-3.5 kgs). In our study, maximum number of
cases of MAS were seen in babies with birth weight between 2.5-2.9kg (n=36,
37.5%), followed by babies with birth weight between 2.0-2.4 kg (n=26, 27.0%).
Babies with birth weight between 3-3.4 formed 16.6% (n=16) of cases. Babies
between 1.5-1.9kg formed 12.5% (n=12), and those 3.5-3.9kg formed 6.2%(n=6). In
our study, female babies were more affected (n=57,59.4%) than males
(n=39,40.6%).
Table 4: Downe s score at admission to MAS
|
Downe s score |
No of Cases of MAS |
Percentage |
|
4 |
26 |
27.08 |
|
5 |
26 |
27.08 |
|
6 |
31 |
32.2 |
|
7 |
8 |
8.3 |
|
8 |
5 |
5.2 |
In this study, with 96
babies of MAS at admission 26 cases (27%) had Downe s score of 4, and 26 cases
(27%) had a score of 5; 31 cases (32.2%) cases had score of 6, 8 cases (8.3%)
had score of 7, 5 cases (5.2%) had score of 8 at the time of admission.
Table 5: APGAR score at 1 minute in MAS cases
|
APGAR Score |
No Cases of MAS |
Percentage |
|
0-3 |
2 |
2.08 |
|
4-6 |
79 |
82.29 |
|
>6 |
15 |
15.62 |
Out of all cases, 2
(2.08%) cases had severe asphyxia i.e., AS ≤ 3 at 1 minute and 79
(82.29%) cases had mild to moderate asphyxia i.e., AS between 4-6 at 1 minute
and Apgar score > 6 is seen in 15 (15.62%) cases.
Table 6: Complications in MAS
|
Complication |
No of cases of MAS |
Percentage |
|
HIE 2 |
35 |
36.4 |
|
HIE 3 |
8 |
8.3 |
|
Sepsis |
55 |
57.2 |
|
Shock |
16 |
16.6 |
|
DIC |
3 |
3.1 |
|
Meningitis |
3 |
3.1 |
|
AKI |
9 |
9.3 |
|
Hypoglycemia |
8 |
8.3 |
|
Jaundice |
9 |
9.3 |
|
PPHN |
7 |
7.2 |
|
Pneumothorax |
5 |
5.2 |
|
No complications |
7 |
7.2 |
Sepsis was seen as the
most frequent complication (n=55,57.2%) followed by HIE 2 (n=35,36.4%) and
shock(n=16,16.6%). Less frequent complications were acute kidney injury (AKI),
jaundice, hypoglycemia, pneumothorax, PPHN.
Table 7: Mortality in MAS
|
Most attributable cause |
No of deaths |
|
Pneumothorax |
5 |
|
Sepsis |
6 |
|
PPHN |
4 |
|
HIE 3 |
3 |
|
HIE 2 |
1 |
|
DIC |
2 |
Most of the mortality is
due to sepsis (n=6,28.5%), followed by pneumothorax(n=5,23.8%), PPHN(n=4,19%),
and HIE3(n=3,14.2%). HIE 2 and DIC were less frequent causes to be attributed.
It is worth noting that though we have taken the most attributable cause,
multiple factors are contributing to deaths in most cases.
Table 8: Neurological Outcomes in MAS
|
Neurological Status |
No of Cases of MAS |
Percentage |
|
Abnormal Neurological examination at
discharge/death |
38 |
39.5 |
|
Normal neurological examination |
58 |
60.4 |
In our study, 58(60.4%)
newborns had a normal neurological examination at the time of discharge, as
assessed by Amiel Tison system of neurological assessment. Rest of them
(n=38,39.5%) had depressed reflexes owing to the effects of birth asphyxia.
Table 9: Correlation between APGAR at 1 minute and
mortality
|
Outcome |
Apgar<7 |
Apgar>7 |
p-value* |
|
Death |
21(25.9%) |
0 |
0.026 |
|
Discharge |
60(74.1%) |
15 |
- |
*Pearson s Chi Square
test
APGAR Score at the time
of birth seems to correlate with the outcome of MAS patients. Those having
score of <7 had significant mortality than those with score>7. Analysis
was done using Pearson chi-square test, showing a p-value of 0.026, which is
statistically significant.
Table 10:
Correlation between Respiratory distress and mortality
|
Outcome |
Downe s<5 |
Downe s>5 |
p-value* |
|
Death |
0 |
21 |
0.022 |
|
Discharge |
26 |
49 |
- |
*Pearson s Chi Square
test
Downe s Score at the
time of admission were compared and analyzed using Pearson chi square test.
Significant mortality was seen in the group having score ≥ 5, with
p-value of 0.02, thus was statistically significant.
DISCUSSION- Out of the 5460 admissions that were registered
during the study period, 4892 (89.5%) of the infants had trouble breathing.
Among them, 96 experienced meconium aspiration syndrome (MAS), with a meconium
aspiration fluid (MSAF) prevalence of 12.3%, and 780 (15.9%) were born with MSAF.
This frequency closely matches the results of Swain et al.'s 1987 study, which
showed 13.92% MSAF and 8.5% MAS. Between 1.7% and 35.8% of these individuals
have MAS, according to studies that report a prevalence of MSAF ranging from
5.6% to 24.6% [7,8]. Within the reported range, the current study's
MSAF and MAS prevalence is quite acceptable.
Meconium staining and
subsequent MAS were found to occur more frequently in deliveries linked to
prolonged labour (26%), hypertension (22.9%), and maternal anaemia (19.8%) in
the current study. We compared these incidence rates with other writers' reports.
According to research by Coughtrey [9] newborns that have
respiratory distress during MSAF frequently experience foetal distress. The
prevalence of pregnancy-induced hypertension (PIH) was reported to be 11.20% by
Rahman et al. [10], 15.75% by Argyridis and Arulkumaran [11],
and 23.58% by Gallo et al. [12], In this investigation, 22.9%
of the participants had PIH. It was discovered that the incidence of premature
rupture of membranes (PROM) was 10.4% as opposed to 6.60% in research conducted
by Ayres-de-Campos D et al. [13]. According to Gupta et al.
[14]. meconium passing in postdated pregnancies with oligohydramnios led
to 12.5% in our study.
Significant correlations
have been found between MSAF and small-for-gestation foetal growth status, PIH,
eclampsia, extended rupture of membranes (>24 hours), oligohydramnios,
foetal bradycardia, and foetal tachycardia, according to the National Neonatal
Perinatal Database of India 2002 2003. Research conducted at BHU in Varanasi
and by Hofmeyer GJ and Xu [15] suggested links between MAS and
intrauterine growth restriction (IUGR), heavy meconium staining in amniotic
fluid, and foetal distress during labour. Small-for-gestational-age and IUGR
foetuses made up 47.9% of the population in our study.
In the current study,
the greatest percentage of newborns with MAS were delivered by caesarean
section (53.1%), with normal or aided vaginal delivery (46.9%) coming in
second. These results are consistent with data presented by other writers.
54.2% of babies were born by caesarean section, according to Narang et al.
[16] however, 80% of meconium aspiration cases were linked to
caesarean sections by Bhusan et al. [17].
The current study's mean
gestational age of 38 40 weeks was discovered to be in line with the findings
of Erkkola et al. [19] who discovered that 95% of cases had
gestations longer than 36 weeks. According to Green and Paul101, at 38 weeks,
the prevalence of MAS rises to 10% or higher. Research conducted by Narang et
al., Bhusan et al. and Alchalbi et al. showed that as
gestational age increases, so does the prevalence of meconium-stained amniotic
fluid. [16,18]
Most MAS newborns
(86.3%) in this study showed significant respiratory distress upon entry, as
determined by their Downes score (which ranged from 4 to 6). It has been
observed that many infants with meconium aspiration are relatively well for a
few hours after birth before developing progressive respiratory distress.
George and Goodling106 et al. showed that in puppies, the meconium moves
progressively to the periphery of the lung with each breath.
In the current study,
mild to moderate birth asphyxia was indicated by scores between 4-6 in 82.3% of
cases, while 2% of cases with severe birth asphyxia had APGAR scores reported
at 1 minute ≤ 3. APGAR scores at one minute were found to be less than
seven in 7.5% of instances by Erkkola [19] but Alchalbi et al.
[18] reported scores less than seven in 25.40% of cases.
Sepsis accounted for most
complications in the current study (57.2%), with HIE-2(36.4%), shock (16.6%),
AKI and jaundice (9.3%), hypoglycemia, HIE-3(8.3%), PPHN (7.2%), pneumothorax (5.2%),
DIC, and meningitis (3.1%) following in order. In 7.2% of instances, there were
no extrapulmonary problems. Pneumothorax occurred in 11.53% of infants with
MAS, according to research by Green et al. [20]
CONCLUSIONS- Meconium Aspiration Syndrome (MAS) is a serious
risk to infants, which highlights the necessity of preventative measures. The
illness has prenatal as well as postnatal roots; in the event of foetal
distress, anticipation becomes critical due to the prevalence of maternal risk
factors. Severe cases, which involve intrauterine gasping brought on by hypoxia
and acidosis, probably happen prior to the first breath. To lessen the severity
of MAS, current preventative techniques in the birth room centre on intubating
and suctioning depressed newborns; nonetheless, total prevention is still
unattainable. Still, a major obstacle persists, particularly in developing
nations: the absence of uniform therapy facilities and management practices.
SUMMARY- In summary, negative outcomes can be
considerably reduced by early detection and care based on knowledge of the
maternal and neonatal risk factors connected to meconium aspiration syndrome.
Although enlightening, the study has some drawbacks, including the use of
follow-up data for outborn patients and the possibility of underreporting
details related to resuscitations in delivery rooms. Improving MAS management
and lowering infant mortality need addressing these issues and developing
standardised protocols.
Research concept- Bijayalaxmi Mallick
Research design- Abinashi Sabyasachi
Sethy
Supervision- Satyaranjan Mallick
Materials- Abinashi Sabyasachi
Sethy
Data collection- Bijayalaxmi Mallick
Data analysis and Interpretation- Asmit Shobhan
Behera
Literature search- Satyaranjan
Mallick
Writing article- Asmit Shobhan Behera
Critical review- Asmit Shobhan Behera
Article editing- Asmit Shobhan Behera
Final approval- MaAsmit Shobhan Behera
REFERENCES
1.
Wiswell TE, Bent RC. Meconium staining and the MAS. Pediatr Clin North
Am., 1993; 40: 955.
2.
Meharban Singh (ed). Respiratory Disorders. In: Chapter 19, Care of the
New Born, 6th edition, Sagar Publications, New Delhi. 2004: pp. 263.
3.
Caughey AB, Postterm Pregnancy. Updated: Mar 26, 2021. Available at:
https://emedicine.medscape.com/article/261369-overview?form=fpf.
4.
Okoro PE, Enyindah CE. Time of passage of first stool in newborns in a
tertiary health facility in Southern Nigeria. Niger J Surg., 2013; 19: 20-22.
5.
Addisu D, Asres A, Gedefaw G, Asmer S. Prevalence of meconium stained
amniotic fluid and its associated factors among women who gave birth at term in
Felege Hiwot comprehensive specialized referral hospital, North West Ethiopia:
a facility based cross-sectional study. BMC Pregnancy and Childbirth, 2018; 18:
429. doi: 10.1186/s12884-018-2056-y.
6.
Nath GDR, Penchalaiah A. Study of clinical profile of meconium
aspiration syndrome in relation to gestational age and birth weight and their
immediate outcome at Narayana Medical College Hospital, Nellore, India. Int J
Contemp Pediatr., 2017; 4: 2142-50.
7.
Bezboruah G, Chakraborty A, Bhunia N. A Study of Clinico-Epidemiological
Profile of Meconium Aspiration Syndrome in Newborn Admitted in NICU of Gauhati
Medical College and Hospital. Sch J Appl Med Sci., 2016; 4(10A): 3553-56.
8.
Monfredini C, Cavallin F, Villani PE, Paterlini G, et al. Trevisanuto,
D. Meconium Aspiration Syndrome: A Narrative Review. Children, 2021, 8: 230.
doi: 10.3390/children8030230.
9.
Coughtrey H. Possible causes linking asphyxia, thick meconium and
respiratory distress. Obstet Gynecol. 1991; 31(2): 97-102.
10. Rahman S, Unsworth J, Vause S. Meconium in
labour. Obstetrics Gynaecol Reprod Med., 2013; 23(8): 247-52.
11. Argyridis S, Arulkumaran S. Meconium stained
amniotic fluid. Obstetrics Gynaecol Reprod Med., 2016; 26(8): 227-30.
12. Gallo DM, Romero R, Bosco M, Gotsch F, et al.
Meconium-stained amniotic fluid. Am J Obstet Gynecol., 2023; S1158-78. doi:
10.1016/j.ajog.2022.11.1283.
13. Ayres-de-Campos D, Spong CY, Chandraharan E.
FIGO consensus guidelines on intrapartum fetal monitoring:
Cardiotocography. 2015; 131(1), 13 24.
doi: 10.1016/j.ijgo.2015.06.020.
14. Gupta V, Bhatia BD, Mishra OP. Meconium stained
amniotic fluid: antenatal, intrapartum and neonatal attributes. Ind Pediatr.
1996; 33: 293-97.
15. Hofmeyer GJ, Xu H. Amnioinfusion for meconium
stained liquor in labour. Cochrane Database Systemic Rev., 2010; 1: 2.
16. Narang A, Nair PMC, Bhakoo ON, Vashist K.
Management of meconium stained amniotic fluid- A team approach. Indian Pediatr.,
1993;30:9-13.
17. Bhusan PK, Prasad R, Prasad US, Krishna SA,
Gupta NP, Mishra KN, et al. Bihar Pedicon- Conference abstracts. 2006; 9: 3.
18. Alchalbi HA, Abu- Heija AT, El- Sunna E, et al.
Meconium stained amniotic fluid in term pregnancies A clinical review. J
Obstet Gynecol., 1999; 19(3): 262-64.
19. Erkkola R. Meconium aspiration syndrome. Ann
Chir Gynecol Suppl., 1994; 208: 106-09.
20. Green JN, Paul RH. The value of amniocentesis in
prolonged pregnancy. Obstet Gynecol., 1998; 51(3): 293-98.