Exclusion Criteria- Cases
excluded from the study are given below:
1. Plasmacytoma
and Multiple Myeloma, Hairy cell leukemia, Hairy cell leukemia variant,
Prolymphocytic leukemia.
2. Disagreement
between the provisional light microscopic diagnosis and final diagnosis after
immunohistochemistry.
3. Cases
with limited biopsy specimen, insufficient material, poor fixation and staining
pattern.
Cases
where no paraffin blocks were available for further study.
Data Collection- Age,
sex, site of biopsy, clinical information, all investigative parameter results
were captured through Hospital Information System (HIS).
Of the total 115 cases which were provisionally
diagnosed as various subtypes of lymphoma on light microscopy with hematoxylin
and eosin staining supported by PAS (Periodic shiff’s
staining) and Reticulin staining are retrospectively analyzed by two
independent pathologists. All the cases were subjected to immunohistochemical
staining and analyzed. Long battery of markers are
used according to the primary morphology which includes CD45, CD20, CD3, C5,
CD10, CD30, CD7, CD23, CD43, CD15, CD30, CD56, CD4, CD8, CD7, Bcl2, Bcl6,
Cyclin D1, Tdt, EMA, CD99, CD117, PAX 5, Alk 1. Non
lymphoid markers were also used in differentiation with other round cell tumors
like AE1/AE3, CK7, CK20, TTF, Synaptophysin, HMB-45, Calcitonin, Thyroglobulin,
Vimentin etc.
Statistical
Analysis- The continuous data were summarized in
Mean, median and range whereas discrete (categorical) in number (n) and
percentage (%). Data was tabulated and compared and Pie chart was made.
Ethical Approval- This
diagnostic study was approved by Institutional review board. The committee
waived the informed consent to the participants in view of retrospective nature
of study with review of records only.
Four cases were not further followed up
due to insufficient material, poor staining and fixation and five cases could
only be diagnosed as non-Hodgkin’s lymphoma as the paraffin blocks were already
being issued to the patients thus were excluded from the study. Thus total 104
cases were finally selected. Distribution of lymphoid neoplasm, patient
demography, age range, median age, male to female ratio, nodal and extra nodal
site distribution is shows in Table 1.
Table 1: Epidemiological and
Histological distribution of cases
|
|
Lymphoma Subtypes |
No |
Age (yrs) |
Sex |
Site |
% |
||||
|
Range |
Median |
Male |
Female |
M:F |
Nodal |
Extra nodal |
||||
|
|
Non Hodgkin lymphoma |
89 |
77(8-85) |
52.5 |
58 |
31 |
1.87:1 |
43(48.3%) |
47 (52.8%) |
85.5% of total |
|
A |
Precursor lymphoid neoplasm T cell lymphoblastic lymphoma |
2 |
8( 4-12) |
10 |
0 |
2 |
- |
1 (50%) |
1 (50%) |
2.24% |
|
B |
Mature B-cell neoplasm |
|
|
|
|
|
|
|
|
|
|
1 |
Chronic lymphocytic leukaemia/small
lymphocytic lymphoma |
1 |
58 |
- |
1 |
- |
- |
1 |
- |
1.12 % (NHL) |
|
2 |
Splenic Marginal Zone Lymphoma |
2 |
4(65-69) |
67 |
0 |
2 |
- |
- |
2 |
2.24% (NHL) |
|
3 |
Extranodal marginal zone lymphoma of mucosa associated lymphoid
tissue (MALT Lymphoma) |
4 |
28 (43-71) |
61 |
2 |
2 |
1:1 |
- |
4 |
4.49 % (NHL) |
|
4 |
Follicular lymphoma |
3 |
20 (50-70) |
57 |
3 |
- |
|
3 |
- |
3.37% (NHL) |
|
5 |
Mantle cell lymphoma |
1 |
79 |
|
1 |
|
|
1 |
- |
1.12% (NHL) |
|
6 |
Diffuse large B-cell lymphoma (DLBCL), NOS |
47 |
59(26-85) |
55 |
35 |
12 |
2.9:1 |
29 (61.7%) |
18 (38.3%) |
52.8% (NHL) |
|
7 |
Primary diffuse large B cell lymphoma of CNS |
14 |
49(26-75) |
53 |
8 |
6 |
1.3:1 |
- |
14 |
15.7% (NHL) |
|
8 |
Extranodal marginal zone lymphoma of mucosa associated lymphoid
tissue of the dura |
1 |
45 |
- |
- |
1 |
- |
- |
1 |
1.12% (NHL) |
|
9 |
T cell/histiocytic –rich B cell lymphoma |
1 |
50 |
- |
- |
1 |
- |
1 |
- |
1.12% (NHL) |
|
C |
Mature T- and NK- cellneoplasms |
|
|
|
|
|
|
|
|
|
|
1 |
Extranodal NK/T- cell lymphoma, nasal type |
2 |
15(15-30) |
22.5 |
- |
2 |
- |
- |
2 |
2.24% (NHL) |
|
2 |
Intestinal T-cell lymphoma (monomorphic epitheliotropic intestinal T cell lymphoma ) |
1 |
30 |
- |
- |
1 |
- |
- |
1 |
1.12% (NHL) |
|
3 |
Hepatosplenic T- cell lymphoma |
1 |
42 |
- |
1 |
- |
- |
- |
1 |
1.12% (NHL) |
|
4 |
Peripheral T-cell lymphoma, NOS |
6 |
39(33-72) |
55.5 |
5 |
1 |
5:1 |
5 |
2 |
6.74% (NHL) |
|
5 |
Angioimmunoblastic T-cell lymphoma |
2 |
4(42-46) |
44 |
1 |
1 |
1:1 |
2 |
- |
2.24% (NHL) |
|
6 |
Anaplastic large cell lymphoma, ALK Negative 1 |
1 |
45 |
- |
1 |
- |
- |
- |
1 |
1.12% (NHL) |
|
|
Hodgkin lymphoma |
15 |
60(7-67) |
20 |
9 |
6 |
1.5:1 |
12 |
3 |
14.4% (Total) |
|
|
TOTAL |
104 |
|
|
|
|
|
|
|
|
Among the included patients, 15 (14.4%) patients were
diagnosed as Hodgkin’s lymphoma while 89(85.5%) were belong to Non-Hodgkin lymphoma group. As the focus of the study was
non-Hodgkin’s lymphoma, further Hodgkin’s lymphoma categorization was not
evaluated. Majority of NHL were mature B-cell neoplasm (n=74, 83.1% of NHL),
while mature T-cell and NK cell neoplasm were less (n=13, 14.6% of NHL).
Precursor lymphoid neoplasm were rarely found in only two cases (n=2, 2.24%).
On further categorization of NHL, most common subtype found was Diffuse large
B-cell lymphoma (DLBCL, n=47, 52.8%) followed by Primary diffuse large B cell
lymphoma of CNS (CNS DLBCL, n=14, 15.7%). Peripheral T-cell lymphoma, NOS
(PTCL, NOS, n=6, 6.74%), extranodal marginal zone
lymphoma of mucosa associated lymphoid tissue (MALT lymphoma, n=4, 4.49%),
Follicular lymphoma (FL, n=3, 3.37%), Splenic marginal zone lymphoma (SMZL, n=
2, 2.24%), Angioimmunoblastic T-cell lymphoma (AITL, n=2, 2.2-24%) were in
decreasing order of frequency. Anaplastic large cell lymphoma (ALCL), Chronic
lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), Mantle cell lymphoma
(MCL), T cell/Histiocytic-rich B cell lymphoma (THRLBCL), Intestinal T cell
lymphoma (MEITL), Hepatosplenic T-cell Lymphoma (HSTL) each seen in one patient
only (n=1,1.12%).
Male outnumbered females in both non-Hodgkin and
Hodgkin lymphoma. In non-Hodgkin male to female (M/F) ratio was1.87 while in
Hodgkin lymphoma it was 1.5. Median diagnosis age for NHL is 52.5(8-85) years
while for HL it is 20 (7-67) years. Commonest subtype DLBCL, NOS showing median
age 55 (26-85) years and male to female ratio 2.9: 1, while CNS DLBCL revealed
median age 53 years (26-75) and male to female ratio 1.3:1. Among the most
common T- cell lymphoma, PTCL, NOS median age was 55.5 years and male to female
ratio 5:1.
In this study 54 cases were showing primarily lymph
node involvement (51.9%) while 50 cases showed extranodal
involvement (48%). Nodal involvement is common in Hodgkin’s lymphoma (80%),
while in non-Hodgkin’s lymphoma it was seen in 60.6 % cases only. Distribution
in term of nodal and extranodal site is show in Table
2 and Fig. 1.
Table 2: Distribution of cases nodal vs extranodal
|
|
Lymphoma site |
Number |
Percentage |
Age (Yrs) |
Sex |
|||
|
|
|
|
|
Range |
Median |
Male |
Female |
M:F |
|
A. |
Nodal |
54 |
51.9% |
|
|
|
|
|
|
B |
Extra nodal |
50 |
48.0% |
|
|
|
|
|
|
1 |
Central nerous
system Brain - 14 Frontal- 4 Parietal-3 Temporal- 2 Corpus callopsum-2 Third ventricular, thalamic,
Posterior fossa- one each Meninges-1 |
15 |
30% of extranodal 14.4% of total |
49(26-75) |
53 |
8 |
6 |
1.3:1 |
|
2 |
Gastrointestinal tract Stomach 9 Small intestine 1 Large intestine 1 |
11 |
22% of extranodal 10.5% of total |
41(30-71) |
45 |
8 |
3 |
2.7:1 |
|
3 |
Testis |
5 |
10% of extranodal
4.8% of total |
20(57-77) |
70 |
5 |
- |
- |
|
4 |
Spine |
7 |
14% of extranodal 6.7% of total |
20 (50-70) |
39 |
4 |
3 |
1.3:1 |
|
5 |
Breast |
2 |
4% of extranodal 1.9% of total |
1(44-45) |
44.5 |
- |
2 |
- |
|
6 |
Thyroid |
1 |
2% of extranodal 0.9% of total |
60 |
|
|
1 |
|
|
7 |
Urinary bladder |
1 |
2% of extranodal 0.9% of total |
26 |
|
1 |
|
|
|
7 |
Orbit |
1 |
2% of extranodal 0.9% of total |
69 |
|
|
1 |
|
|
8 |
Mediastinum
|
4 |
8% of extranodal 3.8% of total |
37(8-45) |
22.5 |
1 |
3 |
1:3 |
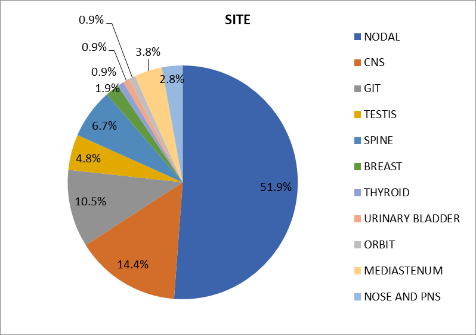
Fig. 1: Pie chart showing
lymphoma cases according to site of involvement
Most common extranodal site was CNS seen in 15 cases (n= 15/50, 30%)
followed by GIT (n=11/50, 22%). Involvement of spine was third most common (n=
7/50, 14%). Among the primary CNS lymphoma, Frontal region was the most common
site (4/15,26.6%) followed by Parietal region (3/15, 20%) temporal region
(2/15, 13.3%) and corpus callosum (2/15, 13.3%). Third ventricular, thalamic,
posterior fossa involvement were seen in one case each (n=1, 6.6%). Median age
was 53 years with age ranged from 26 to 75. Maximum (8 cases) seen in fifth
decade of life.
Among
the primary GIT, Gastric lymphoma is seen in 9 cases, out of which DLBL seen in
5 cases, MALT lymphoma in 3 cases while one case of 45 yrs
male with histomorphological features of high-grade
lymphoma labeled as Anaplastic large cell lymphoma- ALK negative.
Primary
testicular lymphoma was seen in 4.8% of all NHL and 10.0% of extranodal lymphoma with mean age of 67.8 years and age
range from 57-77 years. Four cases were of unilateral involvement while one
patient with B/L involvement left > right with paratesticular,
soft tissue and spermatic cord and inguinal lymph node metastasis.
Primary
B cell NHL involving thyroid, urinary bladder, orbit, breast are
found while nose and paranasal sinuses were primarily involved by T- Cell NHL.
Out of three cases of primary mediastinal involvement two were diagnosed as
T-cell Acute lymphoblastic lymphoma, while one is primary mediastinal B-Cell
NHL.
Table 3: Distribution of
Non-Hodgkin’s lymphoma in various studies from India, China and US
|
Arora et al.
[5] n=4026% |
Mondal et al.
[6] n=455% |
Gogia et al.
[7] N=390% |
Meng et al.
[8] n=2027% |
Al-Hamadani et al. [9] N=596476% |
Present study N=89% |
|
|
DLBCL |
46.9 |
35.2 |
68.5 |
41.3 |
32.5 |
52.8 |
|
EN/NK T CL |
0.9 |
- |
1.3 |
13.4 |
- |
2.24 |
|
MALT |
2.4 |
2.0 |
2.3 |
8.0 |
8.3 |
4.49 |
|
FL |
10.5 |
19.3 |
9.0 |
6.6 |
17.1 |
3.37 |
|
MCL |
1.6 |
2.6 |
5.0 |
4.0 |
4.1 |
1.12 |
|
AITL |
1.4 |
1.4 |
0.75 |
3.6 |
- |
2.24 |
|
CLL/SLL |
4.1 |
5.5 |
1.3 |
3.5 |
18.6 |
1.12 |
|
PTCL,NOS |
5.9 |
1.7 |
3.85 |
2.9 |
1.7 |
6.74 |
|
ALCL |
5.1 |
12.1 |
1.8 |
2.2 |
1.0 |
1.12 |
DLBCL: Diffuse large B-cell lymphoma,
EN/NK T CL: Extranodal NK/T cell lymphoma, MALT:Extranodal marginal zone
lymphoma of mucosa associated lymphoid tissue, FL: Follicular lymphoma, MCL:
Mantle cell lymphoma, AITL: Angioimmunoblastic T- cell lymphoma, CLL/SLL: Small
lymphocytic lymphoma, PTCL, NOS: Peripheral T-cell lymphoma, not otherwise
specified, ALCL:Anaplastic large cell lymphoma.
DISCUSSION-
The incidence of lymphoma increasing steadily over the last two decades.
According to International agency for Research on Cancer; Globocan
Non-Hodgkin’s lymphoma (NHL) affecting 2.8% of all new cases of cancer
worldwide with mortality of 2.6% of all cancer death while Hodgkin lymphoma
(HL) is affecting 0.44% of new cancer cases with death percentage of 0.27%
globally. Incidence in India is almost similar to world figure. Here NHL
comprises of 2.7% of all new cancer cases with mortality in 2.4% of all cancer
deaths annually while HL seen in 0.59% of new cancer cases with mortality in
0.41% of cases of cancer death.[6]
Numerous studies worldwide showed a
higher median age for Non-Hodgkin lymphoma in western
population in comparison with Asian figures. In India the median age for NHL is
only almost a decade less than western figures. In our study the median age of
NHL is 52.5 years similar to other studies from India. [1,7,8] However
the males outnumbered the female in both western and Indian figures.
Distribution and comparison from various types of Non-Hodgkin lymphoma on histology from various studies from
India, China and US. [9-13]
In the present
study DLBL is the most common subtype seen in 52.8% of cases in concordance
with other studies but the sticking difference here is low incidence of
follicular lymphoma and a much higher incidence of Primary DLBCL of CNS. Low
rate of FL in this study and also in the developing countries might be due to
late detection of cases and DLBCL might progressed from previously undiagnosed
FL. [14] Higher incidence of Primary DLBCL of CNS should be more
widely searched and studied in comparison with overall neurosurgery patients
and surgically resected neurosurgical specimens.
Lymphoma are also being classified clinically as nodal
or extranodal type. Extranodal lymphoma, by
definition, involves sites other than lymph nodes, spleen, thymus and the
pharyngeal lymphatic ring. Involvement of the spleen in HL is considered as
nodal disease but in the case of non-Hodgkin lymphoma (NHL) the spleen is
regarded as an extranodal site.[15] Extranodal involvement is more common in NHL than HL.
In the present study Primary extranodal
lymphoma was seen in 48% of cases. The key defining criteria used here as when
the extranodal site is the only site of disease or
the bulk of disease is confined to extranodal sites. There is a changing
trend of extranodal lymphoma now a days due to
increasing usage of immunosuppressive therapy, indolent viral infection and
HIV.[13] Most common extranodal site
involvement was seen as head and neck region or GIT in previous studies. [17,18]
In the present study Central nervous system (CNS) is
the most frequent site for extranodal lymphoma, seen
in 30% of all cases of extranodal lymphoma. This is
in contrast to the previous literature where it has been described as only 4-6%
of all extranodal lymphoma.[18] The median
patient age and localization is in concondrance with
previous studies. [19] All of the cases belong to diffuse large B-cell lymphoma of
the CNS and confined to brain except for one case which was arising from dura.
Second common extranodal
site in our study is GIT, seen in 20% of cases of extranodal
lymphoma. This incidence is almost similar to the previous studies. DLBCL was the
most common histologic type in GIT comparable to observations made by studies
from India and other parts of the world. [20,21] The second common
histologic type found was ENMZL/MALT lymphoma.
CONCLUSIONS- Lymphoma
at a glance in a single tertiary care hospital revealed higher incidence of NHL
over HL. Median age of NHL is almost a decade less than western figures and
male outnumbered female. DLBCL is the most common subtype, however incidence of
FL and CLL/SLL are less. Primary extranodal lymphoma
belongs to 48% of cases and CNS being the most common extranodal
site followed by GIT. Causes for this
must be meticulously searched. The major limitation of the present study was
inherited selection bias because the cases collected from single institution
where major bulk of cases belonging to neurosurgery, gastroenterology and
nephrology. Pediatric population catered by the hospital is less, and the
patient’s population is also from surrounding states.
This is just an attempt to overview the lymphoma in
the population of this region, which was getting unnoticed since inception.
CONTRIBUTION OF AUTHORS
Research
concept- Anju Shukla
Research
design- Anju Shukla
Supervision-
Anju Shukla
Materials-
Poonam Singh
Data
collection- Surbhi Gupta,
Poonam Singh, Priyanka Jain
Data
analysis and Interpretation- Anjika Shukla,
Poonam Singh
Literature
search- Anju Shukla
Writing
article- Anju Shukla, Anjika
Shukla
Critical
review- Poonam Singh,
Priyanka Jain
Article
editing- Anjika Shukla
Final approval- All Authors
REFERENCES
1.
Nair R, Arora N, Mallath MK. Epidemiology of
lymphoma in India. Oncol., 2016; 91S (1): 18-25.
2.
Suveillance, Epidemiology, and End Results Program. Cancer
Stat Facts: Non-Hodgkin Lymphoma. National Cancer Institute. https://seer.cancer.gov/statfacts/html/nhl.html.
3.
Swerdlow
SH, Campo E, Harris NL, Jaffe ES, Pileri SA, et al.
WHO Classification of Tumours of Haematopoietic
and Lymphoid Tissues. Rev 4th ed., Lyon; IARC, 2017.
4.
Armitago JO, Gascoyne RD, Lunning MA, Cavalli F.
Non-Hodgkin lymphoma. Lancet, 2017; 390(10091): 298-310.
5.
Sun R, Medeiros L, Yong K. Diagnostic and
predictive biomarkers for lymphoma diagnosis and treatment in the era of
precision medicine. Mod Pathol., 2016; 29: 1118-42.
6.
Sung H, Ferlay J, Siegal RL, Laversanne
M, Soerjomataram I, et al. Global cancer statistics
2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin., 2021; 71(3): 209-49. doi:
10.3322/caac.21660.
7.
Prakash G, Sharma A,
Raina V, Kumar L, Sharma MC, Mohanti BK: B cell non-
Hodgkin’s lymphoma: experience from a tertiary care center. Ann. Hematol., 2012; 91: 1603-11.
8.
Sandhu DS, Sharma A,
Kumar L. Non- Hodgkin’s lymphoma in Northern India: An analysis of clinical
features of 241 cases. Indian J Med Pediatr Oncol.,
2018; 39(1): 42-45.
9.
Arora N, Manipadam MT, Nair S. Frequency and distribution of
lymphoma type in tertiary care hospital in south India: analysis of 5115 cases
using World Health Organization 2008 classification and comparison with world
literature. Leuk Lymphoma, 2013; 54: 1004-11.
10. Mondal
SK, Mandal PK, Samanta TK, Chakaborty S, Roy SD, et
al. Malignant lymphoma in Eastern India. A retrospective analysis of 455 cases
according to World Health classification. Indian J Med Pediatr
Oncol., 2013; 34(4): 242-46.
11. Gogia
A, Das CK, Kumar L, Sharma A, Sharma MC, et al. Profile of non- Hodgkin
lymphoma: An Indian perspective. South. Asian. J Cancer, 2018; 7(3): 162.
12. Meng
J, Chang C, Pan H, Zhu F, Xiao Y, et al. Epidemiological characteristics of
malignant lymphoma in Hubei, China: A single-center-5-year retrospective study.
Med., 2018; 97(35): e12120.
13. Al-Hamadani
M, Habermann TM, Cerhan JR, Macon WR, Maurer MJ, et
al. Non-Hodgkin lymphoma subtype distribution, geo-dermographic patterns, and survival in the US: A
longitudinal analysis of the National Cancer Data Base from 1998 to 2011. Am J Hematol., 2015; 90: 790-95.
14. Mahanta
D, Sharma JD, Sarma A, Kakoti L, Kataki AC, et al. Pattern of T-cell
non-Hodgkin’s lymphoma in a tertiary care center in North East India. Indian J
Med Paediatric Oncol., 2019; 40(3): 391-95.
15. Gurney KA, Cartwright
RA. Increasing incidence and descriptive epidemiology of extranodal
non-Hodgkin lymphoma in parts of England and Wales. Haematol J., 2002;
3: 95–104.
16. Guermazi A, Brice P, de Kerviler EE, Fermé C, Hennequin
C, et al. Extranodal Hodgkin disease: spectrum of
disease. Radiographics, 2001; 21: 161–79.
17.
Das
J, Ray S, Sen S, Chandy M. Extranodal involvement in
lymphoma-A Pictorial Essay and Retrospective Analysis of 281 PET/CT studies.
Asia Ocean J Nucl Med Biol Spring,
2014; 2(1): 42-56.
18. Schlegel U. Primary CNS lymphoma. Ther Adv Neurol Disord., 2009; 2(2): 92-104.
19. Decked
M, Paulus W, Kluin PM, Ferry JA. Lymphoma. In: Louis
DN, Ohgaki H, Wiestier OD,
Cavenee WK, Ellison DW, Branger DF, editors. WHO Classification of Tumours of the Central Nervous System. 4th ed.
Lyon: IARC Press; 2017; pp. 272-77.
20. Otter
R, Bieger R, Kluin PM, Hermans J, Willemze
R. Primary gastrointestinal non-Hodgkin’s lymphoma in a population-based
registry. Br J Cancer, 1989; 60: 745-50.
21.
Ghimire P, Wu GY, Zhu L.
Primary gastrointestinal lymphoma. World J Gastroenterol., 2011;
17(6): 697-707.