INTRODUCTION- The term
mucocele appendix was coined by Karl Freinherrvon Rokitansky in 1942 [1-3].
Mucocele appendix is an obstructive disorder, resulted due to an extra
proliferation of epithelial tissues of the abdominal region, which result in
the appendix dilation because of intraluminal accumulation of mucilaginous
fluids. But it is a rare disorder. The reported incidence of this disorder was
0.2% to 0.7% only from appendectomy specimens [4-6]. The
frequency of the disease equally appeared in both the sex, as observed between
the 5th and 7th decades of life [7].
Mucocele appendix is further classified into four types according
to the histopathological examinations: a) Retention cyst, b) mucosal
hyperplasia, c) mucinous cystadenoma and d) mucinous cystadenocarcinoma [8].
But the worst thing about this disorder is lack of initial sign of
appearance, only diagnosed when this disease approaches to its advanced level.
It means mucocele appendix doesn’t have any clinical sign of appearance.
Sometimes, a patient with appendiceal
mucocele have feel pain in a lower right quadrant of the abdomen; that’s
why mistakenly diagnosed as acute appendicitis. If untreated or misguided, then
mucocele symptoms may be appeared in the peritoneal cavity, ultimately it
transformed into a dangerous form of the disease called pseudomyxoma peritonei,
which has a high mortality rate [8]. Its more advanced
form is termed as Jelly belly Syndrome [9] in which peritoneal
cavity has only mucinous like fluids. The main objective of the current study
is to investigate the appendiceal lesions, through the USG as a primary
diagnostic tool. Instead of this, an extensive preoperative investigation, and
their diagnosis in a patient with appendicitis disorder remains a difficult
task, but detectable only at the time of surgery.
CASE PRESENTATION- The present study is a case of 46-year-old person, who was suffered from
chronic appendicitis admitted in the
Department of Emergency, GSVM Medical
College, Kanpur to confirmation of
appendicitis in an admitted patient had found abdominal pain at the lower right
portion, nausea, fever and vomiting like symptoms are also reported.
These reported symptoms appeared at 4 months prior and then again
sub-sided after medicine intake, but the treatment is not perfect because the
same symptoms appear 2 days prior repeatedly and the condition of the admitted
person has become worse, that’s why that person must undergo for further
medical checkup by the surgeon and if the symptoms like palpation tenderness
was noted at Mcburneys point, abdominal muscles appeared to moderately rigid
and rebound tenderness, then it is serious. For more confirmation, the patient
body temperature was regularly checked, its measured temperature is 37.8°C and
total leucocyte count, (TLC), 14400 cells/mm3 was noted. From
abdominal USG images confirmed the loops of the intestine puffed with the gases
in the lower right region of abdomen. After diagnosed the patient with acute
appendicitis, should undergo open appendectomy, a surgical removal of the
appendix. An observed area of the swollen appendix would be 4x3x2 cm, noted at
the time of surgery. At the swollen portion of the appendix, a cystic mass
(1x0.8x0.7 cm) of fluids was appeared with no perforation. No free fluids were
accumulated in the peritoneal cavity of the stomach. A fluid like mucin is
accumulated at the inflamed portion of the appendix, medically it is known as
mucocele of the appendix was diagnosed. Thus, the appendectomy surgery must be
followed due to cystic mass of fluids is appeared only at the tip instead of
the based region of the appendix. But the stage of appendicitis has not
appeared chronic it may be at acute stage due to the following reasons: Size of
lymph nodes is not increased. There was no complication in the postoperative
period. Specimens send for histopathological examination in the pathology
department. For histopathological examination, grossly specimen received in one
labelled vial mentioned as appendix. A piece of tubular tissue was taken as
specimen of 4x3x2 cm diameter. The tissue collected from the appendicular tip
has thickened globular area of 1x0.8x0.7 cm. The tissue collected have outer
surface which is smooth and shiny with fibro-fatty adhesions with attached
mesentery, it’s one end is open and the other end is closed. For further study
of the thickened globular area, this is expected to have mucoid like fluid.
Microscopy Fig. 1 and Fig. 2
reveals appendiceal mucosal mucinous hyperplasia, there is cystic dilatation of
lumen. Lumen shows mucinous secretion. There is mild inflammatory cell
infiltrate in the layers of the appendix. These Microscopic findings are
suggestive of appendiceal mucocele with chronic appendicitis.
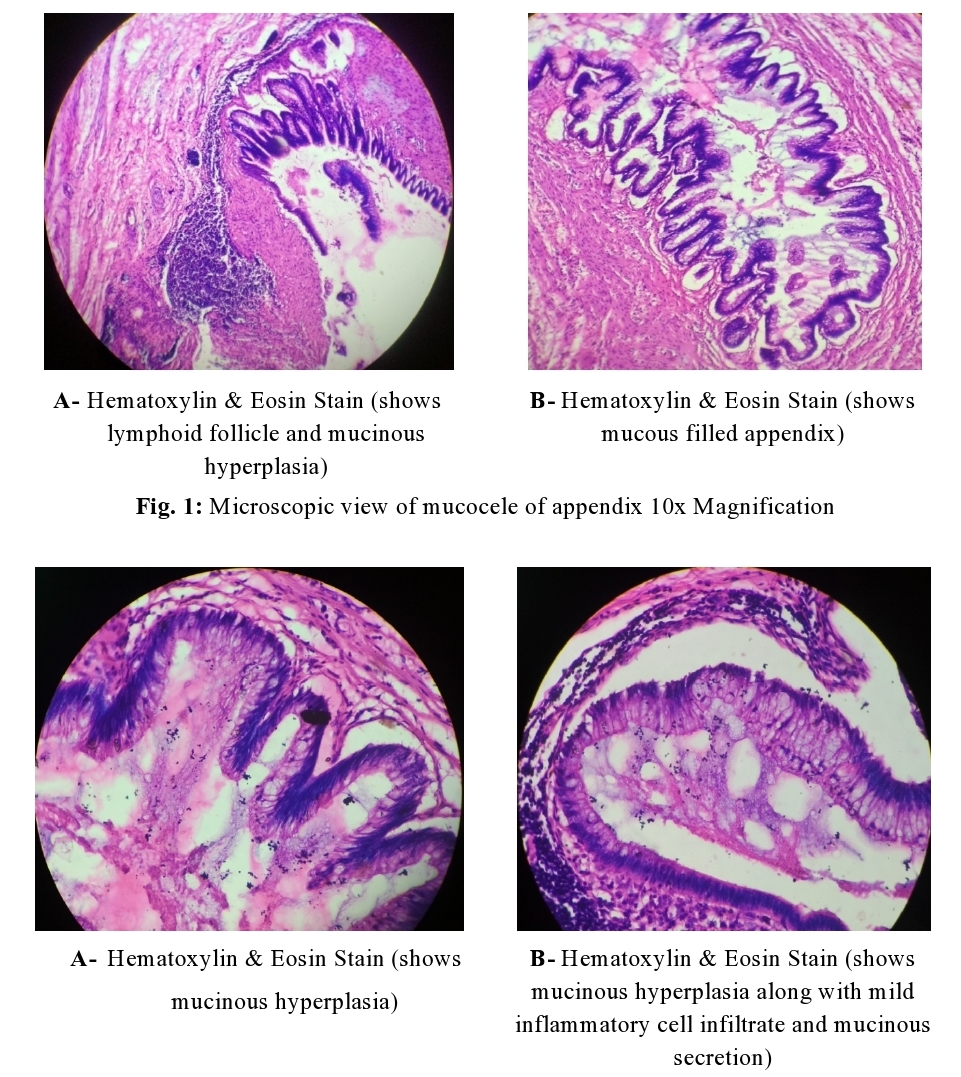
Fig. 2: Microscopic view of mucocele
of appendix 40x Magnification
DISCUSSION- Mucocele of the
appendix is a bulged portion of appendix by mucous following the mucinous,
mucinoma cystadenoma (63%), mucosal hyperplasia (25%), mucinous
cystadenocarcinoma (11%), ultimately result in retention cyst mass formation [10].
The basic reason for mucocele occurrence is due to the lumen blockage by
endometriosis or carcinoid tumour at the specified location. Approximately, 50%
appendicitis cases were observed while examinations
through radiological method or by following the surgical methods. Most studies
reported to confirm its prevalence among women, while some studies also
demonstrate its higher incidence among men [11,12].
Appendiceal mucocele classification is based on histological
features of lumen obstruction [13].
1. Simple mucocele (Inflammatory,
obstructive, or retention cyst)– Blockage
and inflammation in appendicular epithelial tissues were resulted due to
destruction in epithelial cells but no incidence of hyperplasia or mucosal
atypia was reported.
2. Hyperplastic Mucocele- An
abnormal growth of appendicular tissues inside the lining of the colon which
results in appendix dilations.
3. Mucinous cystadenoma- It is an appendix neoplasm with dysplastic epithelium proliferation, similar to colon
adenomatous polyps.
4. Mucinous cystadenocarcinoma- It is a abnormal growth and
proliferation results called cellular dysplasia with stromal invasion, besides
having muscular i.e. mucosae.
The most common clinical sign includes extreme pain in the lower
right portion of appendicular tissues, which resulted in bowel habits or
inflamed mass such as diarrhea, constipation, or narrowing of the stool [14]
as observed in rectal bleeding and sign of intussusceptions of the
intestinal colon. Preoperative diagnosis, a surgical method, of appendicular
mucocele is crucial so as, to prevent from peritoneal dissemination,
intra-operative and post-operative complications and repeated surgery [15,16].
USG, or CT and Colonoscopy are commonly used for diagnostic purposes of
appendicitis. This USG methodology is preferable imaging procedure in a patient
with acute abdominal pain. With the help of USG, it can be easy to distinguish
mucocele and acute appendicitis conditions. The distinguishing pattern can be
observed closely increase of acute appendicitis, that is based on the threshold
size of the outer diameter of the appendix is approx. 6 mm, while it will be
more increase of mucocele, also described Receiver operative characteristics
(ROC), showing (83%) sensitivity and (92%) specificity, it means USG defined
the disease diagnosis with good reproducibility and appendicitis is at
prominent stage [17-20]. In addition, CT is considered
the most reproducible and reliable method of diagnostics in this case study. As
compared to USG, following CT method is more preferable because its diagnostic
capacity to detect the mucocele disorder is higher. Symptoms like cystic
dilatation and wall calcification appeared, if the appendix lumen size is
>1.3 cm, and enlargement of appendiceal cavity takes place with the
liberation of yellowish mucous from the cavity, that can be easily visualized
through the colonoscopy.
CONCLUSIONS- This study concludes that the appendiceal
mucocele is easily comparable to acute appendicitis. Preoperative diagnosis is
preferable, an important surgical methodology to prevent severe intra-operative
and post-operative complications in a patient with acute appendicitis.
Ultrasonography and computed tomography are the two best-known methods utilized
for this purpose.
The viewpoint of the study, focus on those patients with age of
>45 year, who suffers from acute appendicitis must undergo for CT and open
surgery instead of following laparoscopic surgery.
CONTRIBUTION OF AUTHORS
Research
concept- Prof. Mahendra Singh, Dr. Jaivijay
Tiwari
Research
design- Dr. Jaivijay Tiwari
Supervision- Prof. Mahendra Singh, Dr. Neelima
Verma
Materials- Dr. Jaivijay Tiwari
Data
collection- Dr. Jaivijay Tiwari
Data
analysis and Interpretation- Prof.
Mahendra Singh, Dr. Jaivijay Tiwari
Literature
search- Dr. Jaivijay Tiwari
Writing
article- Dr. Jaivijay Tiwari
Critical
review- Prof. Mahendra Singh
Article
editing- Dr. Jaivijay Tiwari
Final approval- Prof. Mahendra Singh
REFERENCES
1.
Ferraz de Campos FP. The
Dawn of Modern Pathology. Autops Case Rep., 2016; 6(1): 1–5.
2.
Rokitansky CF. A Manual of Pathological Anatomy, Vol
2, Blanchard & Lea,
Philadelphia, Pa, USA, 1855.
3.
Demetrashvili
Z, Chkhaidze M, Khutsishvili K, et al. Mucocele of the appendix: case report
and review of literature. Int Surg., 2012; 97(3): 266–69.
4.
Rangarajan
M, Palanivelu C, Kavalakat AJ, Parthasarathi R. Laparoscopic appendectomy for
mucocele of the appendix: Report of 8 cases. Indian J. Gastroenterol., 2006; 25
(5): 256–57.
5.
Marudanayagam R, Williams
GT, Rees BI. Review of the pathological results of 2660 appendicectomy
specimens. J Gastroenterol., 2006; 41(8): 745–49.
6.
Tovar RJ, Teruel DG,
Gastineires VM, Dehesa As, Quindos PL, et al. Mucocele of the appendix. World J
Surg., 2007; 31(3): 542-48.
7.
Smeenk RM, van Velthuysen
ML, Verwaal VJ, Zoetmulder FA. Appendiceal neoplasms and pseudomyxoma
peritonei: A population based study. Eur. J. Surg. Oncol., 2008; 34(2):
196–201.
8.
Sugarbaker PH. Appendiceal
epithelial neoplasms and pseudomyxoma peritonei, a distinct clinical entity
with distinct treatments. In: Bland KJ, Buchler MW, Csendes A, Garden OY. Saar
MG, Wong J (eds). General Surgery. Principles and International Practice. London-Limited:
Springer, 2009; 885-93.
9.
Moran BJ, Cecil TD. The
etiology, clinical presentation, and management of pseudomyxoma peritonei. Surg
Oncol Clin N Am., 2003; 12(3): 585–603.
10. Higa E, Rosai J, Pizzimbono CA, Wise L. Mucosal hyperplasia,
mucinous cystadenoma, and mucinous cystadenocarcinoma of the appendix. A
re-evaluation of appendiceal mucocele. Cancer, 1973; 32(6): 1525–41.
11. Ruiz-Tovar J, Teruel DG, Castiñeiras VM, Dehesa AS, Quindós PL, et
al. Mucocele of the appendix. World J Surg., 2007; 31(3): 542–48.
12. Kim SH, Lim HK, Lee WJ, Lim JH, Byun JY. Mucocele of the appendix:
ultrasonographic and CT findings. Abdom Imaging, 1998; 23(3): 292–96.
13. Kumar S, Jasujab P. Appendiceal mucocele-A rare case report. Int J
Surg Case Rep., 2019; 58: 21–25. doi: 10.1016/j.ijscr.2019.04.008.
14. Simon S. Signs and Symptoms of Colorectal Cancer [Internet].
February 18, 2020. Available from:
https://www.cancer.org/latest-news/signs-and-symptoms-of-colon-cancer.html.
15. Aho AJ, Heinonen R, Laurén P. Benign and malignant mucocele of the
appendix. Histological types and prognosis. Acta Chir Scand., 1973; 139(4):
392–400.
16. Sugarbaker PH. Appendiceal epithelial neoplasms and pseudomyxoma
peritonei, a distinct clinical entity with distinct treatments, in: K.J. Bland,
M.W. Buchler, A. Csendes, O.Y. Garden, M.G. Saar, J. Wong (Eds.), General
Surgery. Principles and International Practice. Springer, London-Limited, 2009,
pp. 885-93.
17. Dhage-Ivatury S,
Sugarbaker PH. Update on the surgical approach to mucocele of the appendix. J
Am Coll Surg., 2006; 202(4): 680–84.
18. Lien WC, Huang SP, Chi CL, et al. Appendiceal outer diameter as an
indicator for differentiating appendiceal mucocele from appendicitis. Am J
Emerg Med., 2006; 24(7): 801–05.
19. Francica G, Lapiccirella G, Giardiello C, et al. Giant mucocele of
the appendix: clinical and imaging findings in 3 cases. J Ultrasound Med.,
2006; 25(5): 643–48. doi: 10.7863/jum.2006.25.5.643.
20. Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiol.,
2000; 215(2): 337–48. doi: 10.1148/radiology.215.2.r00ma24337.
21. Sasaki K, Ishida H, Komatsuda T, et al. Appendiceal mucocele:
sonographic findings. Abdom Imaging. 2003; 28(1): 15–18. doi: 10.1007/s00261-001-0175-8.