Int. J. Life. Sci. Scienti. Res., 4(2): 1707-1712,
March 2018
Tuberculosis Among Household
Contacts of Multidrug-Resistant Tuberculosis Cases at a Tertiary Hospital
in Lucknow, India
Rajeev Kumar1*,
RAS Kushwaha1, Amita Jain2,
Zameerul Hasan1, Priyanka Gaur3, Sarika Panday1
1Department
of Respiratory Medicine, King George’s Medical University, India
2Department
of Microbiology, King George’s Medical University, India
3Department
of Physiology, King George’s Medical University, India
*Address
for Correspondence: Mr. Rajeev Kumar, PhD Scholar, Dept. of Respiratory
Medicine, King George’s Medical University, UP, Lucknow, India
ABSTRACT- Background: Multidrug-resistant
tuberculosis (MDR-TB) is caused by strain of Mycobacterium tuberculosis, it is
transmitted through air droplets from infected person and Close contacts of
MDR-TB patients have a high potential to developing TB. This study aims to
determine the profile of TB/multidrug-resistant TB (MDR-TB) among household
contacts of MDR-TB patients.
Material
and Methods: The cases were recruited
from the King George’s Medical University, Lucknow, India. In this
cross-sectional study, Close contacts of MDR-TB patients were screened for
tuberculosis. clinical, radiological and bacteriological experiments were
performed to find out the evidence of TB/MDR-TB.
Results: The
cases were enrolled Between December 2015 to December 2016, a total of 100
index MDR-TB patients were recruited which initiated on MDR-TB treatment. A
total of 428 contacts who could be studied, 11 (2.57%) were diagnosed with
MDR-TB and 4 (0.93%) had TB. The most frequent symptoms observed in patients
were cough, chest pain and fever.
Conclusions: Tracing
symptomatic contacts of MDR-TB cases could be a high yield strategy for early
detection and treatment of MDR-TB cases to contribute to reduced
morbidity, mortalityand to cut the chain
of transmission of infection in the community. The approach should be
bringing about for wider implementation and dissemination.
Keywords: TB,
MDR-TB, Symptomatic, Household, Transmission
INTRODUCTION-
Multidrug-resistant tuberculosis (MDR-TB) is caused by strain of Mycobacterium
tuberculosis that is resistant to at both isoniazid (INH,
H) and rifampicin (RMP, R) that are two
most powerful 1st line anti TB drugs, it is transmitted through
air droplets from infected person and Close contacts of MDR-TB patients have a
high potential to developing TB.
Because of the emergence of resistant
nature of Mycobacterium tuberculosis strains, tuberculosis adopted more
alarming nature in the form of MDR-TB, is a global occurrence that poses a
serious threat to ongoing national TB control programmes. India accounts for about a quarter of the global TB
burden. Worldwide India is the country with the highest burden of both TB and MDR-TB [1]. There
are an estimated 79,000 multi-drug resistant TB patients among the notified
cases of pulmonary TB each year. According to WHO. In 2016 an
estimated 28 lakh cases occurred and
4.5 lakh people died due to TB.
According to the 2017 World Health Organization
global report, approximately 490000 people were infected by MDR-TB. In
addition, there were an estimated 110,000 people who had rifampicin resistant TB (RR-TB). So the number of
people estimated to have had MDR-TB or RR-TB in 2016 was 600,000 with approximately 240,000 deaths. Almost half (47%) of these cases were in
India, China and the Russian Federation, in which India has highest TB
incidence in Asia [1].
The prevalence of MDR-TB in India is
reported to be around 3% in new cases and 12-17% in retreatment cases [2].
Close contacts of MDR-TB cases are expected to be at increased risk of
developing TB due to intense and/or prolonged exposure to index cases in the
weeks to months before diagnosis and treatment beginning [3].
However, contradictory statistics have emerged from different existing studies
concerning the risk of TB in close contacts of drug-susceptible and MDR-TB
patients. A number of studies have reported a comparable risk of transmission
in the two groups [4–6], whereas others have not [7]..
Global TB Report 2017
released by the WHO, India, along with China and Russia, accounted for almost
of half of the 490,000 multi-drug-resistant TB (MDR-TB) cases registered in
2016, but limited data are available from India
to date on the occurrence of TB/MDR-TB among household contacts of MDR-TB
patients. Contact tracing in general is supposed to provide two functions: (1)
identifies contacts with TB disease so that treatment can be initiated early
when disease is more restricted- this in addition serves to decrease
transmission and (2) identifies high-risk infected contacts who might
assistance from either anticipatory treatment or close surveillance [8].
The objective of our study was to estimate
the incidence of TB in household contacts of MDR-TB patents registered at the
DR-TB center KGMU. Many risk factors that
are associated to development of MDR-TB have been reported among contacts but
have not been concurrently assessed. The present study was carried out to
determine the proportion of household contacts, whodevelop
active TB due to direct transmission from an index case in that household
through the clinical, radiological, and bacteriological profile in household
contacts of MDR-TB patients at a tertiary TB care center in Lucknow.
MATERIAL AND METHODS
Setting and Study
design- A cross-sectional study was conducted at
the Department of Respiratory Medicine King George’s Medical University
DOTS-PLUS center, which covers 24 Districts of
Uttar Pradesh. The study population includes all the house hold contacts MDR-TB
patient registered under categary iv drug
regimen of DOTS-PLUS program at DR-TB centre were recruited from December 2015
to December 2016. A total of 100 MDR-TB cases were recruited for this study
after given inform consent. The study was ethically approved by institutional
ethics comitte. All index cases were retreatment
patients who had unsuccessful treatment with 1st line drug
regimen. The majority were residing in urban slum areas and were of poorer
socio-economic position. After an initial phase of hospitalization of about one
month, all index cases received supervised ambulatory treatment with
second-line drugs.
Screening contact
practice at the hospital- At the DOTS-PLUS center, it was a regular work practice to enquire all index
cases if any there family member had pulmonary symptoms (fever, weight loos,
cough and loss of appetite) suggestive of TB. If any symptomatic family members
were recognized, the index case was encouraged to take the family member for
further examination at the hospital.
The DOTS-PLUS center team
did thorough clinical examination of the symptomatic family member together
with detailed history, physical examination, and laboratory work up as per the
guideline of Revised National Tuberculosis Control Programme. Close contacts
with no active TB disease were monitored carefully for at least two years. It
is more important to careful and close follow-up was encouraged for infants and
children less than 5 years of age because they are more prone to suffer from the
disease. Household contacts with no suggestive signs and symptoms of active TB
were aware regarding the signs and symptoms of TB, about their contact with an
MDR-TB index case and about the significance of seeking treatment immediately
if they develop signs and symptoms of TB disease. Follow up monitoring was done
every 1–2 months. Contacts from Lucknow and nearby places, a team
composed of community health workers and medical officer conducted home visits
after every 1-2 month to trace. Those contacts, who came from
outside Lucknow were motivated to visit the DOTS-PLUS center KGMU after every 1–2 months to undergo the
study investigations.
Data collection- After
obtaining informed consent, a standardized case-report form was filled out for
all contacts of each index patient. Sex, age, weight clinical examination
assessment, radiological assessment, closeness to the index case, bacille Calmette-Guérin (BCG)
scar (presence/absence to assess infection rates among vaccinated and
unvaccinated groups) and any history of TB (pulmonary/extra-pulmonary) were
also recorded.
Socioeconomic status based on education,
occupation and family income were classified by using modified Kuppuswamy scale [9].. Nutritional
status was assessed using the body mass index [10].. Sputum
examination for acid-fast bacilli (AFB) on two early morning samples on 2
consecutive days was carried out in all contacts and in case of any positive
result for sputum microscopy, these cases were referred to Intermediate
Reference Laboratory (IRL) for Xpert MTB/Rif
resistance testing. On confirmation from IRL for Rifampicin resistance
on Xpert MTB, these patients were
registered at DOTS-PLUS to start cat 4 treatments. Those cases with no Rif
resistant to Xpert MTB although positive
for sputum microscopy were referred to respective DOTS centres for registration
and treatment initiation. Tuberculin skin testing (TST) using 5 tuberculin
units (TU) purified protein derivative (PPD) was performed in all contacts and
was recorded after 48-72 h at the study center.
A reading of ⩾10
mm was taken as positive. All contacts were also offered human immunodeficiency
virus and Diabetes testing.
Some of the Contacts that were not
available at the time of home visit for interview, their history were obtained
from the index cases or from other relatives of the family. In the case of
casualty of any contact members because of TB, a history was obtained from the
index patients or from other relatives of the family.
The ‘Index case’ was defined as the first
identified case of MDR-TB in the house. All index cases were confirmed by
sputum culture as having MDR-TB
A household Contact case was defined as
any person who shared the same enclosed living space for least 3 months prior
to the identification of the index case and included spouses, children,
parents, siblings and other family members (uncles, grandfathers, cousins).
RESULTS- Between
December 2015 and December 2016, 100 index patients were reviewed that
were started Anti-tuberculosis treatment. Their demographic profile is
shown in Table 1. Over a 67 (67%) were male and 33% female. 54% index
cases belong to urban and 46% belong to rural areas. Out of 100 index
cases Seven (7%) had previous and Nine (9%) had present
history of tuberculosis and majority of index cases were retreatment patients
that received treatment either of first line anti TB drugs of WHO treatment
category regimen previously. In the study population, 410 (80.7%) were HIV
negative, ninety eight (19.3%) of confirmed MDR-TB index cases were also HIV positive.
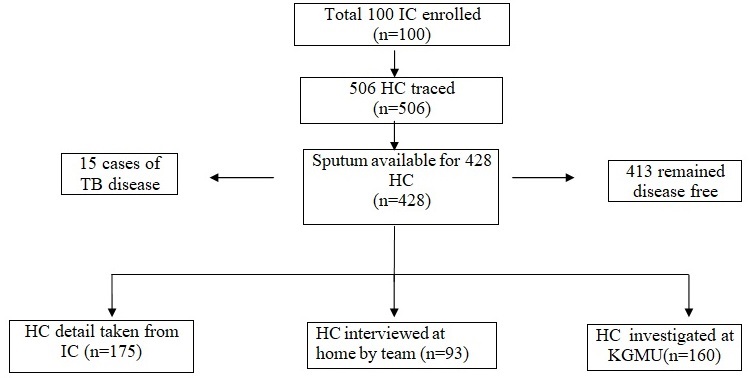
Fig. 1:
Flow diagram representing contact
tracing and outcomes of household contacts
(TB = Tuberculosis, IC= Index
cases, HC= Household contact, KGMU= King George’s Medical University, n= Number
of patients)
Table
1: Socio Demographic characteristics of Index case (IC)
|
Variables |
Frequency
(n=100) |
(%) |
|
Sex Male Female |
67 33 |
67 33 |
|
Age ≤
40 >40 |
58 42 |
58 42 |
|
Residence Urban Rural |
54 46 |
54 46 |
|
Personal
habit Alcoholic Non alcoholic Smoker Ex-smoker Non-smoker |
17 83 27 4 69 |
17 83 27 4 69 |
|
HIV
status Positive Negative |
22 88 |
22 88 |
|
Contact
history Present Past Absent |
7 9 84 |
7 9 84 |
|
Smear
Grading 3+ or 2+ 1+ or scanty |
54 46 |
54 46 |
|
Culture
Result Positive Negative |
98 2 |
98 2 |
The household contacts of the index cases
were identified using the medical records of the index cases that were present
in DR-TB center and through interviews of
index cases and their family members; symptomatic contacts or family members
recognized on the screening form and attached with the respective index case
file.
There were 506 household contacts of 100
index patients were screened for tuberculosis. Their demographic profile is
shown in Table 2. Majority of contacts (67.6%) were male and most of them
(70.4%) belong to the urban area.
Table
2: Socio Demographic characteristics of household contact (HC)
|
Variables |
Frequency
(n=506) |
(%) |
|
|
Sex Male Female |
342 164 |
67.6 32.4 |
|
|
Age ≤
40 >40 |
318 188 |
62.8 37.2 |
|
|
Residence Urban Rural |
356 150 |
70.4 29.6 |
|
|
Personal
habit Alcoholic Non
alcoholic Smoker Ex-smoker Non-smoker |
54 401 94 37 375 |
10.7 89.3 18.5 7.31 74.1 |
|
|
Smear
Grading 3+
or 2+ 1+
or scanty |
(n=15) 11 4 |
73.3 26.7 |
|
|
Culture
Result Positive Negative |
(n=428) 15 413 |
3.50 96.5 |
|
|
Drug
susceptibility testing Resistance Susceptible |
11 4 |
73.3 26.7 |
|
|
Number of
contacts who developed MDR-TB per
household One Two Three |
11 3 1 |
73.3 20 6.7 |
|
Three hundred eighteen (62.8%) of the
contacts have ages bellow to 40 years that are the most susceptible age group
of the population. A symptomatic household contact was identified in 15 of 428
(3.50%) index cases. The most common symptoms were a cough followed by fever
loss of appetite and haemoptysis. History of loss of weight was also present in
all 15 contacts. Sputum specimens were collected and examination was performed
for 428 (83.99%) household contacts, whereas the remaining 78 (15.4%) were
unable to provide sputum for examination. Chest X-ray was performed in 228
contacts. Sputum for AFB yielded negative result for 413 (96.4%) cases while it
was positive in 15 (3.50%), sputum smear positive cases had smear
grading 3+ or 2+ for 11and 1+ or scanty for 4.
All
sputum positive and other suspected cases were referred to Intermediate
Reference Laboratory (IRL) for Xpert testing
and Drug susceptibility testing (DST). Xpert and
DST results of 11 (73.3%) contacts confirmed MDR-TB while 4 (26.7%) was
declared drug-susceptible TB. Four contacts that were diagnosed with pulmonary
TB were referred back to their respective district for registration at
DOTS center for category first whereas the
remaining 11 contacts that were diagnosed as MDR-TB patients were registered
for drug resistant TB treatment at DR-TB center KGMU.
DISCUSSION- In
India, the main objective of National DOTS-Plus Programme is to reduce
tuberculosis transmission by providing early diagnosis and treatment of MDR-TB
patients, for that, it follows the entire protocol of MDR-TB to facilitate
prevention, diagnosis, treatment, and to cover the entire nation with the
scheduling and monitoring in a phased manner. Household
contacts constitute a high-burden group for developing TB and MDR-TB, and the
significance of selective case detection in these groups cannot be
overemphasized. Recently infected contacts carry an eightfold risk of
developing TB compared with persons infected more remotely [11]. While
not all cases found through household contact tracing are the result of
transmission from the index case, early detection and treatment of the
contagious cases will greatly reduce the transmission rate in the
population [12,13]. Because of frequent exposure to index
patient, household contacts of MDR-TB have more recurrent threat to developing
active TB and MDR-TB. On the other hand, available information on subsequent
risk of developing active TB/MDR-TB disease among MDR-TB
contacts have not been reliable. There are very few studies reported
from India on the burden of disease and infection among contacts of MDR-TB
patients. Singla et al reported that TB
prevalence among contacts was 5.3%, of whom only 0.7% had MDR-TB [2]
In
the present study, we measured the factors that are related to contacts such as
residence, any history of TB treatment, HIV status, sex, age, and number of
confirmed MDR-TB in the house. In this study, a total 428 contacts of index
patient studied, of which, 11(2.57%) contacts developed MDR-TB while 4(0.93%)
cases developed drug susceptible TB subsequent to the index case. The Overall
rate of disease in the present study was 3.50 % which is very low as compared
to an earlier study conducted by Dhingra et
al. [14] who reported a 53.5% prevalence of TB
infection in household contacts. We could not determine that household contact
gets infected by transmission from index case as we were not performed genetic
study of mycobacterium. However, as we know it is a communicable disease, there
is significant proof to support the transmission of MDR-TB strain from person-to-person
in the community. It was shown by Bayona et
al. [15] that over half figure of global MDR-TB cases
are thought to result from primary transmission. In addition, the transmission
may have taken place previously, when they were drug-susceptible, as most of
the index cases were retreatment cases. This study had a number of functioning
problems with the simple contact tracing and testing strategies used. Almost a
third of close contacts with cough for more than two weeks
could not provide sputum samples for smear microscopy. While a
number of contacts were unable to produce sputum sample when needed, many
others were simply not present at their home at the time
of visiting the team of DR-TB center.
There are a number of limitations in our study. First, the small sample size of
drug-resistant contact cases due to the inability to trace all the contacts.
Second, data on several determinants for the MDR-TB disease were absent from
analysis because they were not in the routine registers patients. Third, we
considered only household contacts that are living with index patient and not
other casual or close contacts.
CONCLUSIONS- Present
study highlights the requirement for early detection and treatment of TB in
household contacts of MDR-TB, who represent a high-burden group, and also
suggest that active tracing of symptomatic contacts; cases contribute
to reduced morbidity, mortality and transmission of infection in the society.
This could be a very effective approach to saving more people as well as in cutting
the chain of the transmission in the community. The conclusions from this
study are believed to notify the national MDR-TB treatment carrying out plan as
well as other similar countries in their attempt to roll out MDR-TB treatment
services.
ACKNOWLEDGMENTS- We were greatly thankful to Uttar Pradesh Council of Science and Technology (UP-CST), Lucknow for provided funding and department of Respiratory Medicine, King George’s Medical University, Lucknow, India and also appreciates patients participated in this study.
REFERENCES
1.
WHO Global TB Report, 2017.
2.
Singla N, Singla R,
Jain G, Habib L, Behera D.
Tuberculosis among household contacts of multidrug-resistant tuberculosis
patients in Delhi, India. Int J Tuberc Lung Dis, 2011;
15(10):1326–1330.
3.
Centers for Disease Control and Prevention.
Guidelines for the investigation of contacts of persons with infectious
tuberculosis, 2005; 34:1–37.
4.
Teixeira L, Perkins MD, Johnson JL, et al.
Infection and disease among household contacts of patients with multidrugresistant tuberculosis. Int J Tuberc Lung Dis, 2001; 5: 321–328.
5.
Schaaf HS, Vermeulen HA, Gie RP, Beyers N,
Donald PR. Evaluation of young children in household contact with adult
multidrug-resistant pulmonary tuberculosis cases. Pediatr Infect DisJ, 1999; 18: 494–500.
6.
Schaaf HS, Van Rie A, Gie RP, et al. Transmission of multi drug resistant
tuberculosis. Pediatr Infect Dis J,
2000; 19: 695–699.
7.
Siminel M, Bungerzianu G, Anastasaty C. The risk of infection and diseases in
contacts with patients excreting Mycobacterium tuberculosis sensitive
and resistant to isoniazid. Bull IntUnion Tuberc, 1979; 54:
263.
8.
Mulder C, Klinkenberg E, Manissero D. Effectiveness of tuberculosis contact
tracing among migrants and the foreign-born population. Euro Surveill Rev Artic,
2009; 14(11):11.
9.
Kuppuswami B. Manual of socio-economic scale
(urban). New Delhi, India: Manasayan, 1981.
10.
Kuczmarski RJ, Carroll MD, Flegal KM, Troiano RP.
Varying body mass index cut-off points to describe overweight prevalence among
US adults: NHANES III (1988 to 1994). Obes Res
Nov, 1997; 5: 542–548.
11.
American Thoracic Society and Centers for
Disease Control and Prevention. Targeted tuberculin and treatment of
latent tuberculous infection. Am J Respir Crit Care Med,
2000; 161 (4 Pt 2): S221–S247.
12.
Long R, Schwartzman K. Pathogenesis and transmission of tuberculosis.
In: Canadian tuberculosis standards. Vancouver: Canadian Thoracic Society
Canadian Lung Association Public Health Agency of Canada; 2014.
13.
Devadatta S, Dawson JJ, Fox W, et al. Attack
rate of tuberculosis in a 5-year period among close family contacts of
tuberculosis patients under domiciliary treatment with isoniazid plus
PAS or isoniazid alone. Bull World Health
Organ, 1970; 42: 337–351.
14.
Dhingra VK, Rajpal S, Aggarwal N, Taneja DK.
Tuberculosis trend among household contacts of TB patients. Indian J Community
Med, 2004; 29: 44-48.
15.
Bayona J, Chavez-Pachas AM,
Palacios E, Llaro K, Sapag R, Becerra MC. Contact investigations as a means
of detection and timely treatment of persons with infectious
multidrug-resistant tuberculosis. Int J Tuberc Lung Dis, 2003;
7(Suppl 3): S501-S509.