Int. J. Life. Sci. Scienti.
Res., 4(2): 1649-1651, March 2018
Air Ambulance Inter-Hospital ECMO Retrieval of
H1N1 Associated ARDS Patient First of Its Kind Case Reported in India
Gautam Rawal1*, Raj Kumar2, Sankalp Yadav3, Sujana
R4
1Associate Consultant, Respiratory
Intensive Care, Max Super Specialty Hospital, Saket,
New Delhi, India
2Senior Consultant and Incharge, Respiratory Intensive Care, Max Super Specialty
Hospital, Saket, New Delhi, India
3General Duty Medical
Officer-II, Department of Medicine & TB, Chest Clinic Moti
Nagar, North Delhi Municipal Corporation, New Delhi, India
4Infection Control Unit, Max Super Specialty Hospital, Saket, New Delhi, India
*Address for Correspondence: Dr. Gautam
Rawal, Associate Consultant, Respiratory Intensive
Care, Max Super Specialty Hospital, Flat No. 417, Dhruva
Apartments, Patparganj, Delhi, Pin-110092, India
ABSTRACT- Extracorporeal membrane
oxygenation (ECMO) is a revolutionary life-saving technology for patients with
severe but potentially reversible pulmonary or cardiac failure or for patients
in need of a bridge to transplantation. In the Indian scenario, the facility of
ECMO is limited to few specialized healthcare centers having the expertise
personnel and the equipment for this technology. However, the critically unwell
patients with respiratory and/or cardiac failure are managed by all the
healthcare facilities throughout the country. This has led to the development
of mobile ECMO team which carries necessary equipment for initiation of ECMO at
referral center and also retrieval of the patient on ECMO. We present the case
of a patient with H1N1 influenza associated severe ARDS who was retrieved via
air-medical transport (fixed wing aircraft) on ECMO by the mobile ECMO team of
our center. In the present case, the patient was cannulated
and ECMO was initiated at the referral hospital. This allowed a safe transfer
of this patient with severe refractory hypoxemia to ECMO centre. The long or
short-distance inter-hospital transport of critical patients with respiratory
and/or cardiac failure is feasible and safer on ECMO as compared to the
conventional methods of transport. The mobile ECMO teams had made this
technology available to all even when the admitting hospital doesn’t have this
facility and expertise. To the author’s knowledge, this is the first case
reported in India of air-medical retrieval of a patient on ECMO.
Key words: Acute respiratory
distress syndrome (ARDS), Air ambulance, Extra corporeal membrane
oxygenation (ECMO), H1N1 influenza (Swine flu), Hypoxia, Inter hospital
transport
INTRODUCTION- Extra Corporeal Membrane Oxygenation (ECMO) has
seen a remarkable recognition and evolution in its use in the last decade. ECMO
has emerged as an invaluable tool in the hands of intensive care physicians in the
management of patients with severe pulmonary and/or cardiac dysfunction
refractory to conventional management [1], especially in
patients with severe acute respiratory distress syndrome
(ARDS). Though it is not a treatment modality in itself, it serves
as a crucial bridge to therapy in a critical patient, bargaining time for the
treatment or the management to be effective.
In India, ECMO is available only in few specialized centers,
however, the patients with refractory respiratory or heart failure are managed
almost in all intensive care centers throughout the country where this
technology is not feasible or available. Transporting a critical unwell patient
to an ECMO center by the conventional methods can be life threatening and may
cause fatality. This has led to the development of mobile ECMO team (intensivist, anesthetist, or surgeon along with intensive
care nurse and perfusionist) by the few, out of the
many, ECMO centers in India, including our center in Max Super Specialty
Hospital, Saket, New Delhi [2]. Our
ECMO services were established in 2013. The team carries necessary equipment
for initiation of ECMO at a referral center. After the assessment, a final call
is taken by the team if the patient can be transported on conventional
therapies or needs ECMO retrieval. The presented case emphasizes the
feasibility and safety of the inter-hospital transport of the patient on ECMO.
CASE PRESENTATION- A
51‑year‑old obese lady (body mass index 31 Kg/m2) with a
background of hypertension was admitted to Medical Intensive Care Unit (ICU),
in the month of July 2016, of Max Hospital, Dehradun,
Uttarakhand, India (A Hilly Terrain), with bilateral pneumonia and acute
hypoxemic respiratory failure. She was well until six days prior to hospital
admission when she developed fever, cough and progressively increasing
breathing difficulty.
On admission to medical ICU, she was in a
state of severe respiratory distress with tachypnea,
SpO2 of 68% on room air and maintaining 89% on oxygen 10 liters/minute. Her pulse rate was 120/min, with blood
pressure of 80/60 mmHg. She had bilateral crepitations
in chest and rest of the systemic examination was unremarkable, with chest X‑ray
(CXR) showing bilateral non-homogenous infiltrates involving all the four
quadrants of the lung. Septic screening (all cultures) including H1N1 influenza
RT-PCR was sent, and she was empirically started on Piperacillin
+ Tazobactam, Clarithromycin,
and Oseltamivir, along with vasopressor
(norepinephrine) and supportive care. She was put on
non invasive ventilatory support, but she continued
to deteriorate and required endotracheal intubation
and ventilation. Her SpO2 remained low at around 81-85% despite FiO2 of
1.0 and positive end expiratory pressure (PEEP) up to 14 cm H2O,
with arterial blood gas showing PaO2/FiO2 85, pH
7.30, PaCO2 50mmHg suggesting severe ARDS with a Murray score
of 3.5 and dynamic lung compliance of 15ml/cm H2O. In view of refractory
hypoxemia, she was put on prone position ventilation, which initially improved
SpO2 to 92%, but over the next few hours, her SpO2 again
dropped to 82%. ECMO was offered as a possible rescue and therapeutic option,
and a reference was sent to our team for possible transfer to our ECMO center
at Max Super Specialty Hospital, Saket, New Delhi,
India.
ECMO team was mobilized within one hour of the call and was
decided for air-medical retrieval considering the distance, traffic conditions,
the hilly terrain of the referring hospital and the weather. The mobile ECMO
team reached the reference hospital within about three hours of generating the
call. After clinical re-assessment, it was decided to proceed with ECMO
retrieval. Veno-venous ECMO has installed bedside
with 28 F access cannulae in the right femoral vein
and 21 F return cannulae in the right internal
jugular vein via the percutaneous approach by the
team of intensivist and cardio-thoracic surgeon (Fig.1). The procedure was
completed without any complications. ECMO was initiated with settings of flow
rate 60ml/kg/min, speed 3000 rotations/minute, sweep 5litres/minute, fraction
of delivered oxygen of 100% and rest lung ventilation with PEEP 10cm H2O
and peak pressure 25cm H2O. On ECMO support, her SpO2improved
to 98%. She was transported via road-ambulance on ECMO support to the airport,
then in fixed wing airplane (about 45 minutes journey) and then again in road
ambulance to our hospital. A total of about 300 km distance was covered within
a time of 11 hours (including the quick assessment of the patient, cannulation and initiation of ECMO at the referral
hospital). There were no complications during the transport. The patient was
admitted to ECMO ICU at our hospital and continued with the rest lung
ventilation. Laboratory investigations were unremarkable except bronchoalveolar lavage and
nasopharyngeal swab for H1N1 influenza came positive. She showed good initial
recovery with hemodynamic improvement and also improvement in lung compliance.
Unfortunately, she developed secondary bacterial infection with septic shock
and multi-organ dysfunction, on day 8 of ECMO initiation. Her antibiotics were
escalated to Meropenem and Colistin.
However, she continued to deteriorate and started requiring high dose of vasopressors to support her blood pressure and renal
replacement support for acute renal failure and metabolic acidosis.
Regretfully, despite all efforts and support she did not survive and expired on
day 12 of ECMO. An informed consent was obtained for using the clinical images
and the details of the case.
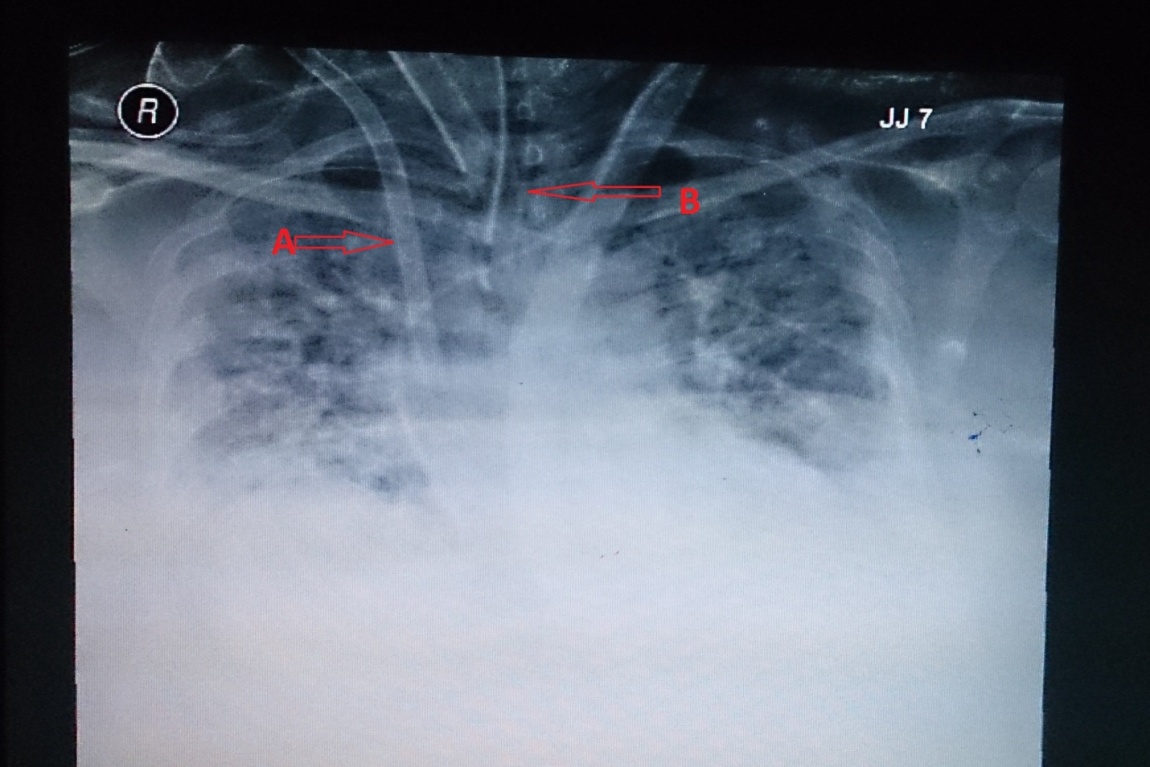
Fig. 1: Chest X-ray showing B/L infiltrates
involving all the four quadrants of the lungs;
A-ECMO canula in Right
IJV; B-Endotracheal tube in situ
DISCUSSION- The development of severe ARDS is a dreaded
complication of H1N1 novel Influenza A viral infection. These patients with
ARDS who do not respond positively with the conventional treatment (prone
ventilation, protective lung ventilation using high PEEP and low tidal volume
of 6ml/kg), are candidates who can be supported by ECMO, which prevents further
organ damage due to hypoxia and acidosis and give sufficient time for the
treatment to have an effect [3]. The technology of ECMO is
ever-evolving and needs the expertise of the healthcare staff for its effective
and uncomplicated use. The scarcity of healthcare personnel with ECMO
experience and the cost of this technology limit its use in India to few major
healthcare facilities in the metropolitan cities.
The transport of these critical patients with ARDS to a
specialized ECMO center becomes a necessity when the patient fails to improve
with the conventional treatment modalities and the cause is potentially
reversible. Occasionally, the patient maybe critically unstable to travel by
the conventional transport and requires the ECMO to be initiated at the local
hospital and then transfer. In our case, the patient had H1N1 associated ARDS
who did not show any signs of improvement and remained hypotensive
and hypoxic for more than 48 hours of using the optimum conventional management
with ventilator. Transport of a patient with ongoing ECMO although remains a
challenge, but has proved to be the only option in some cases which can
increase the patient survival chances by stabilizing the cardio respiratory
failure. The published literature shows various complications while
transporting a patient on ECMO including bleeding, occlusion or breakages of
the circuit, failure of the pump, technical or mechanical complication of the
transport vehicle, etc. [4-9]. In our
case there was no patient complication during transport, which was possible due
to the optimization of the clinical parameters by the multi-disciplined and
experienced ECMO retrieval team which clinically evaluated the patient and
successfully initiated the patient on ECMO at the peripheral hospital.
Unfortunately, the patient could not survive.
Extracorporeal Life Support Organization (ELSO) published
guidelines for transport of patients on ECMO via the three modes of transport
(ground ambulance, helicopter and the fixed wing aircraft) which can be chosen
depending upon the distance, weather conditions, and the availability (Table
1) [6,10].
Table 1: Properties of ground ambulance, helicopter, and
fixed-wing aircraft (from ELSO guidelines)
|
Features |
Ground ambulance |
Helicopter |
Fixed-wing aircraft |
|
Space for team and equipment |
Sufficient (4–5 team members) |
More limited (3–5 team members) |
Variable (≥4 team members) |
|
Noise |
Relatively little |
Very loud |
Loud |
|
Distance for reasonable transport times |
Up to 400 km (250–300 miles) |
Up to 650 km (300–400 miles) |
Any distance |
|
Weight limitations |
Unlimited |
Limited (impacted by distance and weather) |
Variable (depending on aircraft and conditions) |
|
Loading and securing equipment and ECMO circuit/patient |
Relatively easy |
Relatively easy |
Variable (depending on equipment and aircraft model) |
|
Cost |
++ |
+++ |
++++ |
CONCLUSIONS- The ECMO technology has emerged as a savior in
the patients with severe ARDS with reversible cause. The advancement of ECMO
has led to the production of smaller equipment, which can be easily transported
but still require the expertise and facility which is available in the
specialized center. The authors emphasize the development of a mobile ECMO unit
in these advance centers, who can evaluate and initiate ECMO at the referral
hospital and then help in transport of the patient with reduced complications.
The air medical transport has made it feasible for transport across long
distances.
REFERENCES
1. Rawal G, Kumar R, and Yadav S. ECMO Rescue Therapy in Diffuse Alveolar Haemorrhage: A Case Report with Review of Literature. J Clin Diagn Res, 2016; 10(6):OD10-11.
2. Kumar R and Verma D. Inter-hospital
transport of severe acute respiratory distress syndrome on extracorporeal
membrane oxygenation: Extracorporeal membrane oxygenation retrieval. Lung
India, 2016; 33:465-7.
3. Rawal G, Yadav
S, and Kumar R. Acute respiratory distress syndrome: An update and review.
Journal of Translational Internal Medicine, 2016. DOI: 10.1515/jtim-2016-0012.
4. Haneya A, Philipp A, Foltan M, et al. Extracorporeal circulatory systems in the interhospital transfer of critically ill patients:
experience of a single institution. Annals of Saudi Medicine, 2009;
29(2):110-114.
5. Lucchini A, De Felippis C, Elli S, et al. Mobile ECMO team for
inter-hospital transportation of patients with ARDS: a retrospective case
series. Heart, Lung and Vessels, 2014; 6(4):262-273.
6. Broman LM, and Frenckner B.
Transportation of Critically Ill Patients on Extracorporeal Membrane
Oxygenation. Frontiers in Pediatrics, 2016; 4(63):1-6.
7. Broman LM, Holzgraefe B, Palmér K, and Frenckner B. The
Stockholm experience: interhospital transports on
extracorporeal membrane oxygenation. Critical Care, 2015; 19(278):1-6.
8. Isgrò S, Patroniti
N, Bombino M, Marcolin R, Zanella A, Milan M, et al. Extracorporeal membrane
oxygenation for interhospital transfer of severe
acute respiratory distress syndrome patients: 5-year experience. Int J Artif Organs, 2011;
34:1052-60.
9. Ciapetti M, Cianchi
G, Zagli G, Greco C, Pasquini
A, Spina R, et al. Feasibility of inter-hospital
transportation using extra-corporeal membrane oxygenation (ECMO) support of
patients affected by severe swine-flu (H1N1) related ARDS. Scandinavian Journal
of Trauma, Resuscitation and Emergency Medicine, 2011; 19(32):2-6.
10. ELSO. Guidelines for ECMO Transport Ann Arbor: ELSO. Available
from: http://www.elso.org/Resources/Guidelines.aspx, 2015.