Int. J. Life. Sci. Scienti.
Res., 4(6):
2073-2075,
November 2018
Tubercular
Brain Abscess: Diagnostic Dilemma-A Case Report
Areena Hoda Siddiqui1*, Poonam Singh2,
Shilpi Sahai3
1,2Department of Lab Medicine, Sahara Hospital, Viraj
Khand, Gomti Nagar, Lucknow, UP., India
3Department of Respiratory Medicine, Sahara Hospital,
Viraj Khand, Gomti Nagar, Lucknow, UP., India
*Address for Correspondence: Dr. Areena
Hoda Siddiqui, Microbiologist, Department of Lab Medicine, Sahara Hospital,
Lucknow (UP)-226010, India
ABSTRACT- Isolated
central nervous system tuberculosis is uncommon in immunocompetent patients. It
resembles a pyogenic brain abscess clinically and radiologically and poses a
problem in diagnosis and treatment. Here we described a case of recurrent
frontal lobe abscess, which was diagnosed as a tubercular abscess. There was no
clinical or radiological evidence of active tuberculosis elsewhere in the body.
The diagnosis of tubercular abscess was confirmed by
Mycobacterium Tuberculosis by Polymerase Chain Reaction (TB-PCR) in
the abscess material aspirated via a burr hole.
Keywords- Central
nervous system tuberculosis, Frontal lobe abscess, Tubercular brain abscess
INTRODUCTION- The intracranial abscess occurs in 4% - 8% of
Central nervous system- Tuberculosis (CNS -TB) which itself occurs in 10% of
cases of pulmonary TB. It occurs in 20% of
patients who do have HIV infection. Evidence of Isolated CNS-TB is extremely rare occurring in developing countries
and almost always in immunocompromised patients
and can be fatal if undiagnosed [1,2]. Tubercular brain
abscess always poses a diagnostic dilemma as they are hard to distinguish from
pyogenic brain abscesses, tuberculous meningitis, and tuberculoma on the basis
of sign and symptoms, laboratory reports and radiographical presentation. Only
a few cases of Tubercular brain abscess have been reported from India [2,3].
Here we report a successfully treated case of Tubercular brain abscess in
an immunocompetent male.
CASE REPORT- A 40 year old male presented in the neurology OPD
with altered behaviour and headache for the past 10 days. The CT scan taken on
admission showed a left frontal lobe space occupying lesion (SOL). He was
admitted to the neurosurgery department. On admission, the following tests were
performed.
Total leukocyte
count 14.47X109/L; serum urea 12 mg/dl; serum creatinine 0.48 mg/dl;
Viral markers: negative; International normalized ratio (INR) 1.04; Prothrombin
time: 10.1 sec; Activated partial thromboplastin time 19.2 sec; LFT was within normal
limit.
A burr hole drainage was done the next day as shown
in Fig 1. Pus drained was sent to the Microbiology lab for routine culture
sensitivity and Ziehl Neelsen (ZN) smear for Acid fast Bacilli (AFB). The Gram
stain of the pus showed 10-15 pus cells per oil immersion field. No organisms
were seen. The culture was done on Blood agar (Biomerieux), MacConkey agar (MA)
and Brucella blood agar (BBA) (from Oxoid). Pus was inoculated into Robertson
cooked meat (RCM) broth (Hi Media). A second subculture was done from RCM broth
after 5 days on BA and BBA. BBA plates were incubated anaerobically in McIntosh
jar for 48 hours. The culture was sterile after 5 days. No AFB was seen on ZN
staining.
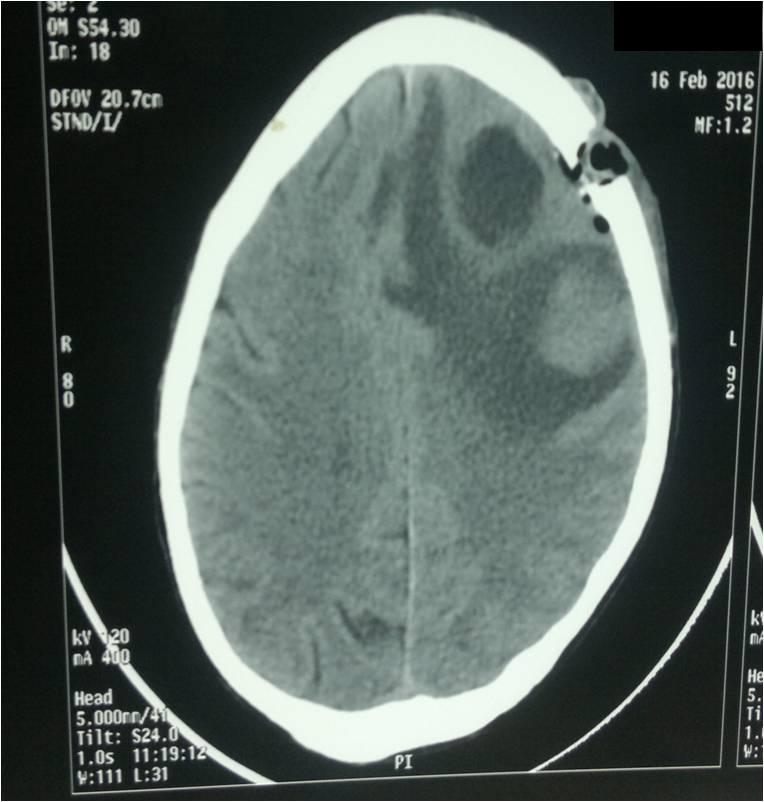
Fig. 1: CT scan showing a burr hole in the frontal
region
He was given
empirical antibiotics, discharged and asked to come for review after a month. A
follow up CT scan after one month showed a SOL again in the frontal lobe. This
time, the pus sample was also sent for TB-PCR (Real Time PCR) at SRL
Diagnostics along with routine culture and sensitivity and AFB smear. For
detection of Mycobacterium tuberculosis complex MTC, Real Time PCR targeting
rpoB gene was standardized using Qiagen DNA Mini Kit [4]. Culture
was sterile after 5 days. A melt curve analysis performed on the Rotor Gene
3000 confirmed the presence of rpoB fragment amplification specific to Mycobacterium tuberculosis.
Anti-tuberculous treatment was then started. All
this time the patient was asymptomatic. Patient was started on Rifampicin 450
mg, Isoniazid 300 mg, Ethambutol 800 mg and Pyrazinamide 1500 mg daily for 2
months. After 2 months, Pyrazinamide and Ethambutol antibiotics were stopped.
Regimen continued for 18 months. Patient recovered successfully.
DISCUSSION- TB
brain abscess can be confused with pyogenic brain abscess as both of them
present acutely with same cerebrospinal fluidCSF abnormalities as happened in
our case. It is difficult to differentiate between pyogenic and tubercular
abscess clinically [5]. Therefore tuberculosis should
always be kept as a differential diagnosis of brain abscess. Patients may
present with features of raised intracranial pressure and focal neurological
deficit commensurate with the site of the abscess. A history of pulmonary
tuberculosis may be present. A relatively long clinical history and an
enhancing capsule with thick wall are suggestive of TBA. Pyogenic abscess,
however, has a thin rim on contrast CT [6]. AFB culture or
nucleic acid detection for smear negative patients should be performed to
reduce morbidity and early initiation of ATT. In cases of recurrent brain
abscess with AFB smear and AFB culture negative, Real time PCR should always be
done to rule out tuberculosis. The high index of suspicion and timely
intervention is required to diagnose and treat this potentially fatal but
easily treatable condition.
CONCLUSIONS- We concluded that M.
tuberculosis is
a rare cause of brain abscess; however, this organism should be considered in
patients with disseminated tuberculosis or in individuals from areas where tuberculosis is endemic and in cases of recurrent brain abscess where AFB
smear and AFB culture is negative, Real time PCR should always be done to rule
out tuberculosis. High index of suspicion and timely intervention is required
to diagnose and treat this potentially fatal but easily treatable condition.
CONTRIBUTION OF
AUTHORS- All the authors have
contributed equally.
REFERENCES
1.
Murthy J.
Multi-drug-resistant central nervous system tuberculosis. Neurol India, 2012;
60: 143-145.
2.
Menon S, Bharadwaj R,
Chowdhary A, Kaundinya D, Palande D. Tuberculous brain abscesses: Case series
and review of literature. Journal of
neuroscience in rural practice, 2011; 2: 153-7.
3.
Sharma V, Newton G. Multiple Tuberculous
Brain Abscesses. Ind. J. Tub, 1992; 39: 185-188.
4.
Kim BJ, Hong SK, Lee KH, Yun, YJ , Kim
EC, Park YG, et al. Differential Identification of Mycobacterium tuberculosis Complex and Nontuberculous Mycobacteria
by Duplex PCR Assay Using the RNA polymerase Gene. J Clin Microbiol., 2004; 42: 1308-12.
5.
Mohindra S, Savardekar A, Gupta R,
Tripathi M, Rane S. Tuberculous brain abscesses in immunocompetent patients: A
decade long experience with nine patients. Neurol India, 2016; 64: 66-74
6.
Kumar R, Pandey CK, Bose
N, Sahay S. Tuberculous brain
abscess: clinical presentation, pathophysiology and treatment (in children).
Childs Nerv Syst., 2002; 18: 118-23.