Key-Words- Retroperitoneal ureterolithotomy (RPUL), Transperitoneal ureterolithotomy (TPUL), Extracorporeal shockwave lithotripsy (ESWL)
INTRODUCTION- Urinary tracts stone disease, which is one of the most common afflictions of modern society, has been described since antiquity. With westernization of global culture the site of stone formation has migrated from the lower to the upper urinary tract and the disease once limited to men has increasingly become gender blind. Until the 1980s, most ureteric calculi that required treatment were managed by open surgical ureterolithotomy or endoscopic basket extraction. Revolutionary advances in the minimally in-vasive and non invasive management of stone disease over the past 3 decades have greatly facilitated the ease with which stones are removed.The advent of extracorporeal shockwave lithotripsy (ESWL), per cutaneous renal surgery and ureteroscopy with endoscopic lithotripsy has almost eliminated the need for open surgical ureterolithotomy. There remains, however, a group of hard core calculi that are poorly treated by minimally invasive means, being stones that are large, hard, long-standing, impacted and in particular those situated in upper or middle ureter. In such cases surgical ureterolithotomy still is necessary, with its con-comitant invasive trauma, major incision, postoperative pain, significant hospital stay and protracted convalescence.
During the last decade laparoscopic surgery has added a further endoscopic minimally invasive option in urology. Since the description of laparoscopic lymphadenectomy[1] and laparoscopic nephrectomy[2] the role of laparoscopy in urology has expanded enormously. A number of different ureteric procedures have been performed including nephro-ureterectomy[3], ureterolysis[4], ureteric resection and repair[5].
This study was carried out to evaluate laparoscopic retroperitoneal ureterolithotomy as a viable option to open surgical ureterolithotomy, laparoscopic transperitoneal ureterolithotomy & endoscopic urology and to assess its place in the spectrum of alternatives for the surgical treatment of ureteric calculi in a tertiary care centre.
MATERIALS AND METHODS- This study was conducted for duration of one year on twenty selected patients of large upper and middle ureteric calculi in the department of General Surgery, Indira Gandhi Medical College, Shimla, India. The objective of this study was to evaluate the efficacy and safety of laparoscopic retroperitoneal ureterolithotomy for management of large upper and middle ureteric calculi on the following parameters. Duration of surgery,CO2 used, Conversion rate to open, Intra-operative complication, Postoperative complication, Hospital stay, Analgesic requirement & Our status as compared to literature.
Operative Technique- All patients were given general anesthesia. A 2cm muscle splitting incision was made just below the tip of 12th rib. The transversalis fascia was incised and the possible para renal space was developed bluntly with a finger. We used a No.7 glove fixed to the end of a No.8 Nelaton catheter as a Balloon dilator. The dilator was placed into the retroperitoneal space under digital control and was inflated with normal saline. After balloon deflation and removal, a10mm Hassan trocar was inserted and a pneumo-retroperitoneum was created withCO2 insufflation. One 10mm trocar was inserted on anterior axillary line 3cm cephalic to anterior superior iliac spine and one 5mm trocar was inserted at the junction of paraspinalis and 12th rib. Three ports were placed on transverse line in preparation for open conversion in case the laparoscopic approach failed. After identifying the ureter on the psoas muscle, the bulge of the stone was located and ureter incised directly over the bulge longitudinally with the cold knife. The stone was removed using a grasping forceps and ureterotomy was closed with 4-0 vicryl using an intra-corporeal suture. Double J stent was placed laparoscopically. Drain was kept through one of the 10mm ports. The drain was removed after the drain output decreased to below 30cc.
RESULTS- The mean age of the patients was 38.30 years. On an average 44.51 litres of gas (CO2) per case was used in this series. No such reports are available regarding the consumption of gas in literature. Mean operating time was 76.60 minutes (Fig 1).
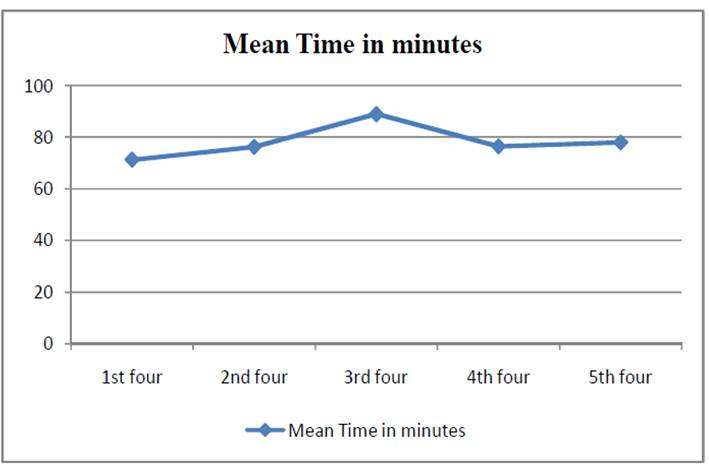
Fig 1: Mean time (minutes) for each case
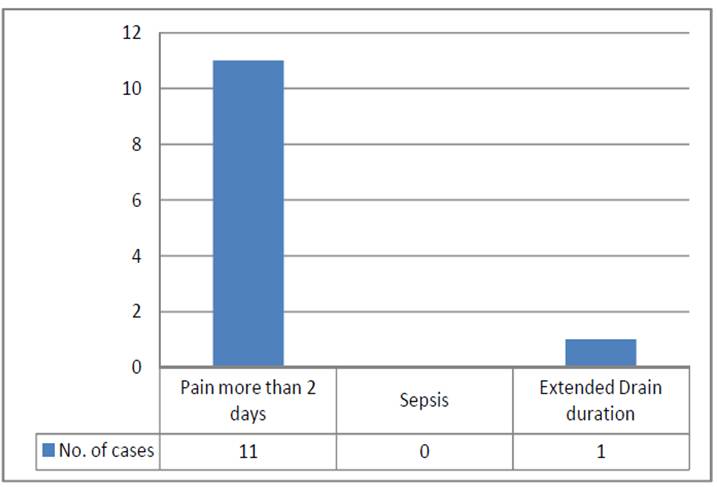
Fig 2: Post operative complications
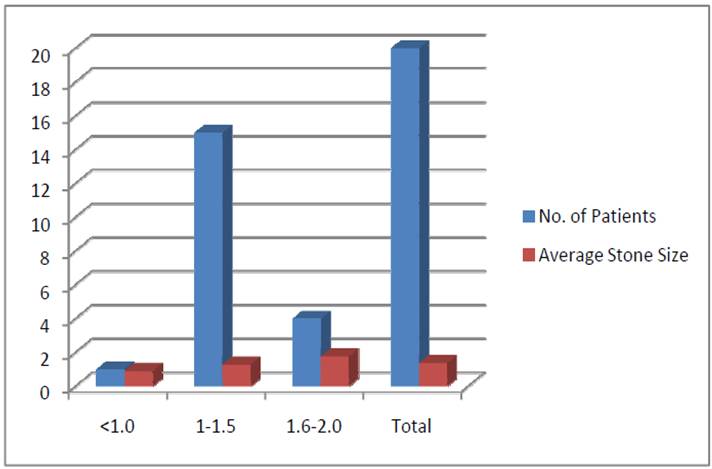
Fig 3: Stone size and average size (cms.)
Pain, Number of Attack and Adhesions- In the present study 100% (20) of patients complained of pain prior to admission. Our evaluation show that presence of adhesions in the patients were related to number of attacks of pain and patients having no adhesions suffered less attacks of pain. Patients with adhesions suffered average 3.83 attacks of pain as compared to patients without adhesion who suffered on an average 3.42 painful at-tacks. The relation between number of attacks of pain and adhesions was statistically significant (P value 0.4210).
Time Taken for Surgery- The mean time taken for completion of the procedure in our series was 76.60 minutes (range 35 to 125 min.). Kwon [6] observed mean operating time of 109 minutes (range 90 to 120 minutes). Tejanshu [7] observed mean operating time of 82 minutes (range 60 to 120 minutes). Gaur [8] had mean operating time of 79 minutes and Goel [9] reported a mean operating time of 108.8 minutes (range 40 to 275 minutes).
However, variation in time taken for surgery in the present cases can be ascribed to the various factors like initial teething troubles, maiden technique, non-availability of trained regular supporting staff familiar with the technique.
Gas (CO2) Consumed- On an average 44.51 litres of gas (CO2) per case was used in this series, ranging from 14 to 80 liters. No such reports are available regarding the consumption of gas in literature [10].
Conversion- In the present series 8(40%) of our cases were converted into open ureterolithotomy. However, there is wide variation in open conversion rate in literature. Jeong [11] observed open conversion rate of 50%. The reason for open conversion in our study was periureteric adhesions, peri-ureteritis and intra-operative bleeding.
Intra-Operative Complications-
Adhesions- Only six of our patients (30%) had multiple peri-ureteric adhesions. Adhesions presented difficulty in dissection during the procedure. All (30%) of them were converted to open surgery. Literature is silent regarding the causes of presence of adhesion.
Spillage of Stone- None of our patients under study had spillage of stone during procedure.
Bleeding- We encountered minor bleeding during procedure in few cases. We encountered major bleeding in one (5%) of our cases. The case was completed by converting to open surgery. It was not a bleeding from any major vessel but probably from increased vascularity due to periureteritis.
Major Vessel and Visceral Injuries- None of our patients sustained these injuries as depicted in literature.
Genito Urinary Injuries- None of our cases encountered bladder or ureteric inju-ries (avulsion) as reported in the literature.
Post-Operative Complications- In the present series none of the patients had wound (port /incision site) infection, abscess formation, prolonged ileus or deep vein thrombosis as reported in literature.
Hospital Stay- There is wide variation in hospital stay as observed in literature. In our series mean hospital stay was 6.65 days.
Postoperative Pain- The mean days of analgesic (Diclofenac) requirement for laparoscopic RPUL were 2.55 days. There is no clear data regarding post operative analgesic requirement in laparoscopic RPUL in lierature.
Post-Operative IVP- All cases in the present series underwent post-operative IVP after a period of six weeks. Only one patient developed postoperative stricture and was managed by open pyeloplasty with DJ stenting. Gaur & Goel all have reported postoperative stricture in their individual case series.
DJ Stenting & Its Removal- DJ Stenting was done in one case of the present series laparoscopically.
CONCLUSION- The increased skills of the surgeons & advances in endoscopic equipment have made laparoscopy the technique of future. In our experience of Laparoscopic RPUL in Indra Gandhi Medical College, Shimla the procedure can be done without any major complication. The minor complications experienced in the study were within the range as reported with the literature. One should have good knowledge of the open ureterolithotomy and if any complication is encountered during RPUL it should be resorted to, as timely conversion of laparoscopy is not a source of shame but sign of wisdom. Time taken for surgery should be no criteria for academic groups. The procedure has definitely shown decreased post-operative discomfort, decreased requirement of post-operative analgesia, better cosmesis, early return to work and less morbidity. RPUL can be considered as another well-established armamentarium in the armour of laparoscopic surgeons and is recommended as an effective minimally invasive primary treatment in large, impacted difficult stones in the upper & mid ureter otherwise indicated for open ureterolithotomy.
REFERENCES
- Schuessler WW, Vancaille TG, Reich H, Griffith DP. Transperitoneal endosurgical lymphadenectomy in patients with localized prostate cancer. J Urol 1991; 145:988-91.
- Clayman RV, Kavoussi LR, Soper NJ et al. Laparoscopic nepherectomy. N Eng J Med 1991; 324:1370-1.
- Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg 1991;1:343.
- Kavoussi LR, Clayman RV, Brunt M, Soper NJ. Laparoscopic ureterolysis. J Urol 1992; 147:426-9.
- Nazet C, Nazhat F, Green B. Laparoscopic treatment of obstructed ureter due to endometriosis by resection and ureteroureterostomy: a case report. J Urol 1992; 148: 865-8.
- Kwon YU, Lee SI, Jeong TY. Treatment of upper and mid ureter stones: Comparison of semirigid ureteroscopic lithotripsy with holmium: YAG laser and shock wave lithotripsy. Korean J Urol 2007;48:171–175
- Shah TP, Vishana K, Ranka P, Patel M, Chaudhary R. : Retroperitoneal laparoscopic ureterolithotomy - our experience. Indian J Urol 2004;20:101-5.
- Gaur DD, et al. Laparoscopic ureterolithotomy: Technical considerations and long-term follow-up. BJU Int 2002;89:339-43.
- Goel A, Hemal AK. Upper and mid-ureteric stones. A prospective unrandomized comparison of retroperitoneos-copic and open ureterolithotomy. BJU Int 2001;88:679-82.
- World Journal of Laparoscopic Surgery, September-December 2009;2(3):47-51, Mark C Cellona St. Luke’s Medical Center, Quezon City, Philippines
- Jeong BC, Park HK, Byeon SS, Kim HH. Retroperitoneal laparoscopic ureterolithotomy for upper ureter stones. J Korean Med Sci. 2006 Jun;21(3):441-4.
| Source of Financial Support: Nil Conflict of interest: Nil |
| International Journal of Life-Sciences Scientific Research (IJLSSR) Open Access Policy Authors/Contributors are responsible for originality, contents, correct references, and ethical issues. IJLSSR publishes all articles under Creative Commons Attribution- Non-Commercial 4.0 International License (CC BY-NC). https://creativecommons.org/licenses/by-nc/4.0/ |