Key-Words- management, Trauma, Paediatric, Intubation
INTRODUCTION- It is most critical in Trauma to immediately restore the airway and quickly establish the life threatening condi-tions. Any delay may be devastating and lapse of each moments need to be accounted in priority.
In trauma patient carrying out quick primary survey and treating the life threatening conditions according to ABCDE is vital. Delayed and inadequate airway management results in devastating consequences.
The airway management of paediatric trauma patient requires a lot of practice/training, thorough understanding of anatomy and Physiology, knowledge and practice of various methods and equipment of airway management, complete and rapid assessment of injuries.
Ineffective management of airway will lead to respiratory failure which in turn may leads to failure of resuscitation. It has been emphasized in various literatures that in-pediatric patient, most cardiac arrest begins as respiratory failure (1-2).
Pediatric patient in contrast to adults have different airway anatomy and physiology which are both unique and challenging. To complicate the situation traumatized kids poses a great challenge to emergency team. It is well documented that lack of proper training in managing the trauma in Pae-diatric in under developed countries is a major cause of fatality. The complexity of the airway management is schematically given in Fig. 1.
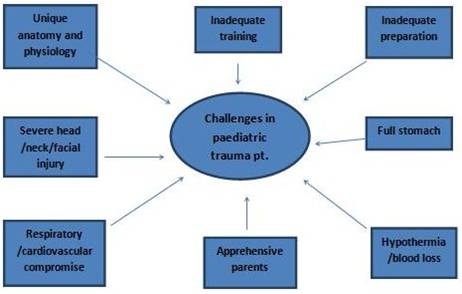
Fig 1: Challenges in airway management in emergency
Anatomical difference-
It is Cleary understood that kids are not small adult (2) and have unique anatomical variation from adult. From birth to adult hood in due course of development of skull, oral cavity, larynx and trachea they have considerable changes in airway anatomy (3). They have large head (3-4) and prominent occiput so when kids lye on flat surface there neck had the tendency to be in flex position (4-5) causing airway obstruction. In order to rectify this variation it is important that shoulder be rolled to keep head in neutral position (4,6-7). Kids have large tongue (4-5,8-10) and adenoids in compari-son to their small oral cavity which causes easy obstruction of airway and difficult laryngoscopy and stabilization of tongue (9). This results into less intra oral visibility and causes suboptimal view of vocal cord. Children Up to the age of five month have obligate nasal breather (4,9) so when there is nasal injury their airway gets compromise. Epiglottis of child is large and omega shape (3) (use of straight blade laryngoscope is advocated), larynx is more rostral/cephaloid (5,10) (anterior placed larynx is misnomer), Vocal cords are more obliquely placed these all causes difficulty in optimum view of vocal card during la-ryngoscopy. The larynx of kids are of funnel shaped in contrast to cylindrical shaped in adult (5,8-9). Recently in vivo measurement by bronchoscopy and MRI images it was consistently found those glottises opening are smaller than cricoid but dispensability of glottis tissue and relative Non-dispensability of cricoid cartilage make cricoid cartilage functionally narrowest part of airway in child (3-4,10).
Physiological difference- Due to high metabolic demand (child have 6 ml/kg oxygen demand verses 3 ml/kg in adult) and low Functional residual capacity (FRC) (3-4,7), when there is compromised state of oxygenation and ventilation, demand and supply mismatch occurs faster in kinds, which leads to early de-saturation (7) and respiratory failure. In children hypoxia leads to bradycardia and hypotension which may leads to cardiac arrest, therefore this sequence of events be broken and prevented as early as possible by pre-venting hypoxia. Further child airway passage are smaller in diameter, hence slight edema or narrowing of airway causes exponential rise in airway resistance and increases in work of breathing(4,9) causes exponential rise of airway.
Assessment of patient- There are certain clinical sign, symptoms and scenario which should alarm us about compromised airway and ventilation in traumatized patients (Table 1-2), a careful evaluation and urgent action plan is lifesaving.
Tachypnea Tachycardia Apnea/hypoventilationChest Indrawing Use of Accessory muscles Wheezing Cyanosis/hypoxia/hypercarbia Level of consciousness/agitation Grunting /stridor Head bobbing |
Severe head injury Severe maxillofacial fractures Risk of aspiration ofblood/vomitus Neck,laryngotrachial injury Chest trauma Severe abdominal injury Severe musculoskeletal injury |
Preparation- Pediatric age group patients have varying shape and size and are of different ages group. Each developing age encounters rapid alterations in anatomy, it thus become imperative to note that one size of equipment does not fit in all. Immediate availability of appropriate size of equipment (Table 3-5) is most essential must otherwise the resuscitation attempts and procedure is bound to fail (5) (for example, Suction, Oxygen, Airway, Pharmaceuticals, Monitor Equipment (SOAP. ME). It is very critical to attach monitor for assessment of all vital parameters and se-cure a good IV line.
Multipara monitor Defibrillator Capnograp Glucometer with strips Automated cell counter Arterial blood gas analyser |
Different size intra venous cannula Infusion sets Intraosseous needle Umbilical vein catheter Central line Syringe Infusion pump with pressure line |
Oxygen delivery system (nasal prong, simple mask, venture mask, mask with reservoir bag) AMBU with oxygen reservoir bag Laryngeal mask airway of various sizes Endotracheal tubes Laryngoscope blade straight and curved Magills forceps Non traumatic Suction catheter Nasogastric tubes of various sizes Difficult intubation cart |
The estimation of fluid requirement and drug dose in growing age is very crucial. A length based resuscita-tion tape such as the Brose low pediatric emergency tape, is an ideal adjunct for the rapid determination of weight based on length for appropriate fluid volume, drug doses and equipment size. (6)
Basic airway management- Most pediatric airway in emergency setting can be handled best with basic airway maneuvers without any further loss of time. First and foremost basic maneuvers are to correct the positioning of patient to clear the airway. It is imperative to follow the cardinal principle and rule of thumb that every trauma patient should be considered to have cervical spine (c-spine) injury (10) unless proved otherwise. The position of head could be maintained in neutral position by placing a roll beneath the shoulder in small children. The obstructed airway could be immediately be opened by performing triple maneuver (head tilt, chin lift and jaw thrust). In suspected c-spine injury head tilt maneuver maybe avoided and patient be placed on spine board with MILS (11).
Oropharyngeal (OPA) and nasopharyngeal (NPA) airway- These adjuncts are used to keep airway patent by displacing tongue or soft palate. OPA is used in unconscious patient who do not have gag reflex (5). Selection of appropriate and precise size of OPA alone is supportive as small size may push the base of tongue further in airway while the large one may obstruct the airway. Oral airway should be gently inserted direct in oropharynx. Insertion of airway backward and rotating 180 degree is not recommended in children as it may cause trauma. NPA could be used in children who do have intact gag reflex with due assessment.
Gentle suctioning with appropriately selected suction pressure can be done to clear the secretion and clots from oral and nasal cavity. It is also essential to ur-gently remove any foreign body, broken tooth to clear the upper airway. Use of Laryngoscopy of appropriate size and Magills forceps may be great advantage for this purpose. After cor-recting the position and suctioning to clear the airways, oxygen therapy commenced immediately (10). Oxygen mask with or without reservoir bag could be utilized depending upon Patient respiratory status.
Reassessment of patient- After basic airway management the patient clinical condition and vitals should be reassessed. Secondary survey of the patient is performed according to ATLS guideline. It is most prudent to evaluate the level of consciousness and adequacy of ventilation and oxygenation need to be examined for further management or need based adjustments. If patient is impending respiratory or cardiac arrest directly immediately bag mask ventilation and intubation be attempted. In trauma patient with head and neck injury feasibility of bag mask ventilation or direct laryngoscopy and intubation would be appropriate.
Bag and mask ventilation (BMV)- BMV is Indicated when the patient spontaneous breathing effort is inadequate despite patent airway. BMV can provide adequate oxygenation and ventilation until definitive airway control is obtained. Proper selection of mask and seal is crucial for effective BMV. Good seal can be obtained by proper holding of mask .If one person performing BMV make C with thumb and index finger over the cup of mask make E with middle finger over the chin, ring finger over the mandible and little finger at angle of mandible(pic ATLS). To make airway patent apply force by middle and index finger whiles at the same time use little finger to push forward the mandible in temporomandibular joint. Do not apply pressure on mask from upward downward because it makes difficulty in opening of mouth. We must attach reservoir bag and oxygen with bag mask assembly and squeeze the bag with other hand. When two people perform BMV one person hold the mask with both hand in same fashion and other person squeeze the bag. Effectiveness of BMV can be assessed by improvement of vitals like heart rate, saturation and improving level of consciousness.
Definitive airway management- When Definitive airway management is mandatory then we look forward for endotracheal intubation to insure uninterrupted ventilation and unwanted obstruction and aspiration. Orotrachial intubation under direct vision with adequate immobilization and protection of cervical spine is the preferred method of obtaining initial airway control (12).
Some of common clinical finding in trauma in children which may require immediate intubation and ventilation are required in children with these clinical sing and finding in Table 6.
Table 6: Some of common clinical finding in trauma in children which may require immediate intubation and ventilation
| S No. | System | Finding | Remark |
|---|---|---|---|
| 1 | Neurology | GCS ≤ 8 | to make airway patent |
| to prevent aspiration | |||
| for controlled ventilation | |||
| 2 | Airway | compromised airway and ventilation | to prevent hypoxemia, hypercapnia and hyperventilation, |
| 3 | Trauma | loss of protective laryngeal reflexes, significant face , neck and thorax injury | burn or smoke inhalation in which oedema may compromise the airway copious bleeding into the mouth from skull base fracture |
Selection of proper endotracheal tube- For quick selection of endotracheal tube we may compare the diameter of tube with child little finger width (13) and the length at which tube is fix is three times the internal diameter if tube (Table 7).
Table 7: ET Tube Size in Pediatric Age Group
| Children >2 years | |
|---|---|
| ETT(UNCUFFED) | 4+AGE/4 |
| ETT(CUFFED) | 3.5+AGE/4 |
| ETT DEPTH (LIP) | 12+AGE/2 CM. |
Confirmation of endotracheal tube placement- No single confirmation technique is completely reliable. Presence of mist in endotracheal tube, bilateral chest movement and equal breath sound especially over axilla, no gastric insufflation sound, ETco2 monitoring are various methods for confirming the correct position of endotracheal tube.
Esophageal detector device, fiber optic bronchoscope, and ultrasonography can be used for confirmation of correct positioning of tube.
After successful intubation ETTshould be secured properly. Till date no literature suggests superiority of any securing devices.
Cuffed vs. Uncuffed- Traditionally, uncuffed tube was preferred in small child younger than 8 years of age (16) because of concern of airway edema, necrosis or stenosis but current literature suggests the use of cuffed tube even in small child especially in trauma patient. Newer cuffed tube is made of thinner material and there cuff is of low pressure high volume type. Cuffed tubes more effectively prevent aspiration and better control of PaCO2 is obtained (16), which is especially helpful in Traumatic Brain Injury. Patient with low compliant lung like ARDS, severe pneumonia, sever burn where higher pressure and minimal gas leak is required for effective ventilation, cuffed tube is preferred. Ideally cuff pressure should be measured as early as feasible and less than 30 mm of Hg is considered safe (5).
After successful intubation if the oxygenation and ventilation worsened consider Displacement, Obstruction of tube, Pneumothorax, or Equipment failure (DOPE) (1).
After securing the ETT make sure head in neutral posi-tion. As child trachea is of small in size (5 cm) when there is flexion, tube can be placed endobronchial or while extension causes misplacement of tube (1).
Rescue devices
Supra glottis airway devices- (14)
Laryngeal mask airway classic
Proseal laryngeal mask airway
Supreme laryngeal mask airway
I Gel
cobra PLA
LTA(laryngeal tube airway)
Air Q
LARYNGOSCOPES- (14)
oxyscope
glidoscope
airtraq
storz DCI
truview PCD infant
bonfils intubation stylet
McGrath
Surgical airways-
Percutaneous crico-thyroidotomy kit
Special concern in trauma- MILS Manual In line Stabilization of neck in trauma patient is important to prevent further neurological damage in suspected c spine injury. In these cases avoid head tilt maneuver, only jaw thrust/chin lift with MILS is applied to open the airway. By MILS we try to keep cervical spine in neutral position. MILS to be continued during transportation, bed shifting, and intubation.
DRUG ASSISTED INTUBATION (DAI)- Previously known as rapid sequence intubation (6). The pertinent details are as under:
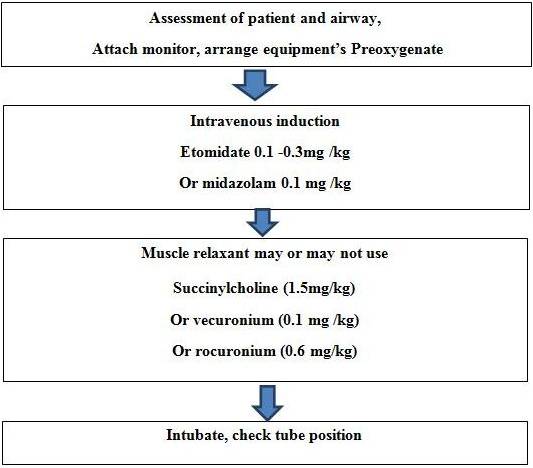
Figure 2: Drug Assisted Intubation
Route- In general we prefer oral route of in trauma cases because of probable injury of basilar skull or cribiform plate. Nasotracheal intubation of more than 24 hours increases probability of sinusitis. Moreover for nasotracheal intubation we choose smaller diameter of tube which causes problem in airway suctioning and increase airway resistance.
Burn- An assessment of degree and type of burns is must to know which patient may need intubation. Below are some common conditions in burn patient which may require intubation.
History of major burn, altered mental status
Circumferential neck burn
Smoke inhalation,
Facial burn, stridor, hoarseness
Soot in the nares or pharynx(6),
Respiratory distress, and Low Spo2 (15).
Early tracheal intubation is considered in these patients. Otherwise ensuing swelling in airway causes airway obstruction and intubation becomes much more difficult later on. Oral intubation with cuffed endotracheal tube is recommended. Special measure for securing the tube is required in severe facial burn like wiring it to maxilla or tying the tape behind head (15). CO poisoning as evident from ABG or some new generation pulse oximeter could treated by giving 100% O2 as it reduces half-life of CO in blood (15-16).
With the help of Bedside fibreoptic bronchoscopy we can assess extent of airway injury (15) and it also allow us to do BAL and suctioning of airway to clear them from shoot, debris or sloughed mucosa (3). Frequent pulmonary toilet as saline lavage and suctioning is required in inhalational injury to prevent obstruction of ETT and worsening of lung parenchyma.
CONCLUSION- Pediatric trauma management is entirely different than adults. The main challenges come from variation in shape and sizes and location of anatomy of airways. Due to various challenges in pediatric airway in emergency situation proper assessment and individualized plan of action is must for effective resuscitation. A trained emergency physician and supporting staff and radially availability of appropriate equipment is key for effective airway management. The main crux in pediatric resuscitation is to prevent hypoxia and break the sequel which may lead to cardio respiratory arrest. A dedicated and highly trained Rapid response team in hospitals may be useful to deal with complexity of pediatrics trauma cases. It also requires decisive and accurate response ability of the team as time is most critical factor. The instruments and equip-ments of various dimensions to suit the various age groups of patients prove very handy in dealing with situation.
REFERENCES
- Special report- paediatric advanced life support: 2016 American heart association guidance for cardio pulmonary resuscitation and Emergency cardiovascular care (e136, e1363, e1364, e1365, e1366).
- R. J. Holm knudsen and L.S. Rasmussen, paediatric airway management, basic aspect, journal compilation, 2008. The acta anaesthesiologica scandinavica foundation date. Acta Anaesthesiologica Scandinavica.
- Cote C J. The difficult paediatric Airway south AFE. J. Anaesthesia analg. 2012, 18 (5): 230-239,231, 232
- Alexander R. Schmidt, markusweiss and Thomas Engelhardt, The paediatric Airwayeur.j. Anaesthesia 2014, 31: 293- 299.
- Advance Trauma Life Support publishing 2016: pp. 250-254.
- BK Rao, vinod k. singh, sumit ray, manjumehra. Airway management in trauma, Indian J. crit. Care med April- June-2004- Vol. 8:2.
- Paediatric guideline, Trauma Emergency in children overview oct. -2006 page 1-5.
- Ronald D. Millerand Lars I. Eriksson, Miller's Anesthesia 7thed., Churchill living stone Elsevier Publishing: 2010: pp. 2562.
- American academy of paediatrics. 126, 5: 2010.
- J. Trauma Acute Care Surg, 73:5, Supplement 4, 2012.
- Jeff harless, Ramesh ramnah and sanjay m bhananker paediatric Airway management Int. J. crit. llln inj. sci 2014, 4 (1): 65-70.
- Kai goldmann. Recent development in Airway management of the paediatrics patientcurr. Opinan aesthesiol 9: 278-284, 2006 Lippincott William s.e Wilkins.
- Bruno Bissonnette Paediatric anaesthesia basic principles state of the art future, ed., 2011 peoples medical publishing house-USA: 2011: pp.1174, 749.
- Francis A. Abantanga Shoa- Ron Jackson, Jeffrey S. upper man Initial assessment andresuscitation of the trauma patient. 27 page- s172-179
- George A. Gregory, Dean B. Andropoulos. Greg-orys paediatric anaesthesia 5th ed., wiley-blackwell publishing: 2012: pp.900, 902.
- Julie Mayglothling, MD, Therese M. Duane, MD, michaelgibbs, MD, Maureen McCunn, MD, MIPP, Eric Legome, MD, Alexander L. Eastman, MD, MPH, James Whelan, MD, and Kaushal H. Shah, MD emergency tracheal intubation immediately following traumatic injury: An Eastern is Association for the Surgery of Trauma Practice management guideline.
- Robert Bingham, Adrian R Lloyd-Thomas, Michael RJ Sury, Hatch and sumners Text book of paedi-atric anaesthesia 3rd ed, 2008.
| Source of Financial Support: Nil Conflict of interest: Nil |
| International Journal of Life-Sciences Scientific Research (IJLSSR) Open Access Policy Authors/Contributors are responsible for originality, contents, correct references, and ethical issues. IJLSSR publishes all articles under Creative Commons Attribution- Non-Commercial 4.0 International License (CC BY-NC). https://creativecommons.org/licenses/by-nc/4.0/ |