ABSTRACT- Alzheimer Disease (AD) is an incurable progressive neurodegenerative disorder. It is the most common
cause of dementia and is increasing worldwide. Various mechanism of pathogenesis of AD is given and is still under
study. Despite of its etiology, the disease is characterized by presence of senile plaques which is deposition of Amyloid
Beta protein and other is intracellular neurofibrillary tangles. Several other factors like Hypertension, diabetes, obesity
and inflammation, hormonal imbalance are associated with increased risk of AD. This article summarizes various
interventions which have impact on slowing the progression of disease therefore any intervention which delays the onset
of moderate to severe symptoms will have significant effect on patient and their families. Also it includes various drugs
and agents which are currently under clinical trial studies. These agents mainly act upon Beta Amyloid, cholinergic
system,various vaccines, antibodies, Y and ß Secretase inhibitors and modulators, Agent affecting phosphorylation and
blocking of tau protein along with agents which have indirect effect on neurotransmission like serotonergic 5HT6,
Histaminergic H3, modulation of acetylcholine response of a-7 nicotinic acetylcholine receptors. Development of new
drugs is very time consuming process and had very less chance of success. The drug which passes the phase 2 clinical
trials with positive results generally fails in phase 3 trial because of serious adverse effect and lack of drug safety profile.
Key-words- Alzheimer, Intervention, ß-Amyloid, Cholinergic
INTRODUCTION-
Alzheimer’s disease is condition in which there is an
irreversible neurodegeneration of brain and protein (1-2). It is
most common form of dementia with progressive
neurodegeneration and impairment in cognition
accompanied by abnormal behavior and personality
changes. With increase in age, chances of the incidences
increase (3). The disease progression is divided into three
stages mild, moderate and severe as determined by global
cognitive test scores. (4)
The pathogenesis of AD is complex and still unclear.
Regardless of its etiology, it is generally accepted that, the
disease is histopathologically characterized by presence of
extracellular neuritic (senile) plagues and intracellular
neurofibrillary tangles.
Due to Accumulation of amyloid B protein (AB), the senile
plaque is formed while the neurofibrillary tangles are made
of hyper phosphorylated tau protein (5). The role of these
proteins in pathophysiology of AD and its relationship with
cognitive symptom is not clear and still under study. For
instance, the amyloid ß (Aß) plaques presences for
identification of AD as distinct disorder, does not clearly
correlate with AD symptom(6) and can be found in healthy
elderly person with sign of no cognitive impairment(7). The
complexity of AD indicates that several other factors are
involved in its pathogenesis.(8) These factors include
genetic makeup that is the incidence of AD in the family of
patient, cerebrovascular disease, traumatic brain injury,
Depression, Hormonal imbalance, Inflammation,
Hyperlipidemia (obesity), Hypertension and Diabetes.
Consumption of high Fat Diet has known to cause increase
risk of number of medical condition including obesity and
diabetes which are associated with increased risk of
Alzheimer disease and other form of cognitive impairment (9-11).
Unfortunately none of therapies are present which
completely stop the progression of disease and there is no
treatment available which intervenes the progressive
deterioration of cognitive and memory functions (12). This
article summarizes various intervention which slows the
progression of disease and the latest advances in anti-AD
Drug candidates which are currently undergoing clinical
trials (1,13-15)
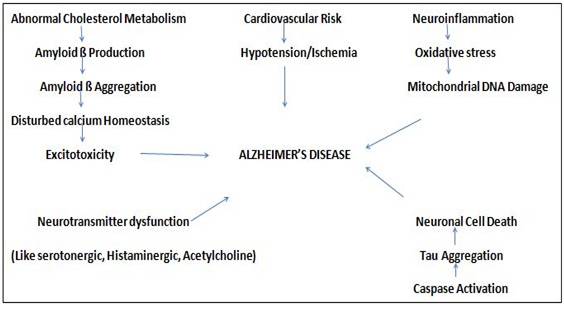
Table 1 : Therapeuticstrategies involve in Alzheimer’s disease3
| 1. | Modulation Of Neurotransmitters |
|
| 2. | Tau Based Therapies Include |
|
| 3. | Amyloid based strategies |
|
| 4. | Oxidative stress reduction |
|
| 5. | Modulation of cellular calcium Homeostasis | |
| 6. | Others |
|
Cholinergic Theory- Multiple neurons are damaged in Alzheimer disease. Most profound damage are in cholinergic system, that is large number of neuron located at the base of forebrain in the nucleus basalis of Meynert, a brain area believed to be involved in thought integration. The discovery of cholinergic cell loss led to the development of cholinergic hypothesis liked to pathophysiology of Alzheimer disease. The cholinergic hypothesis targeted cholinergic cell loss as the main source of cognitive and memory impairment in Alzheimer disease. (16)
Oxidative stress in Alzheimer disease- Oxidative stress is characterized by an imbalance be-tween production of reactive oxygen species and antioxidant defense. With increase in level of ROS, neurodegeneration occur. Another source of reactive oxygen species is amyloid beta peptide itself in presence of metal ions. Therefore oxidative stress is an integral factor in neurodegenerative disease. (16)
Pharmacological treatment For AD- Currently, the treatment Available for AD patient in-clude Acetylcholine esterase inhibitors (AChEIs) and N-Methyl-D-Aspartate (NMDA) receptor antagonist provide at best palliative symptomatic relief of symptoms.
Mechanism of Action of AChEIs- Acetylcholine is the main synaptic and diffuse neurotransmitter of the cholinergic system, a system of complex network connecting limbic and cortical regions involved in control of attention and memory (16). Various cholinergic activity markers such as acetylcholine synthesizing enzyme choline acetyl transferase (ChAT) and receptor binding are decreased in brain of AD patient and have direct effect on cognitive decline (17). AChEIs inhibit the degradation of acetylcholine by acetylcholine esterase thus steady the rate of cognitive decline. Various AChEIs like donepezil, galantamine and rivastigmine are prescribed to AD patient for cognitive aid.
Mechanism of NMDA Antagonist- NMDA Receptor are mainly present in numerous amount at hippocampus and are known for their role in memory formation and learning high plasticity via glutamate neurotransmitter allows the person for long term potentiation. The NMDA are having high permeability to Ca2+ ions but to prevent calcium toxicity, this channel is voltage dependently blocked by magnesium ion thus important for inhibiting neurotoxicity by limiting the high level of Ca2+ influx into post synaptic neuron. Memantine is non-Competitive NMDA Receptor antagonist and able to prevent Ca2+ influx while allowing sufficient Ca2+ necessary for synaptic trans-mission. During convergence of temporal or spatial activation of glutamatergic synapses which occur during learning and memory, the Memantine NMDA receptor channel antagonism is released(18) and used as monotherapy in moderate to severe AD or along with AChEIs.
Effect of Treatment- An effect of AChEIs treatment on cognitive perfor-mance in AD patient has been studied. Double blind placebo controlled studies with Donepezil (5-10mg/kg) found effective in improving cognitive performance in mild-moderate AD (19-20), showing some effect for moderate-severe patient with dose of 23mg/d (21). Small et (22)., (2005) used MMSE to evaluate the effect of oral rivastigmine(8.9 mg/d) treatment for five years, who found decline rate of 8.9 point in treated patient compared to nearly fourteen point in model of untreated patient. In this study, 22.4% of treated patient dropped out due to adverse effect commonly gastric distress. Transdermal patch of rivastigmine reduces these side effects (23) and is clinically effective (24). Also patch may allow patient to receive and maintain the therapeutic dose due to higher retention and compliance (25). Ga-lantamine (18-24mg/d) is well tolerated and provide more protection against cognitive decline when compared with placebo in mild to moderate patient (26). These medications tend to lose their effect once the disease progress beyond the moderate stages and hence these drugs are not licensed for severe AD. AChEIs treatment only target to slow the natural pro-gression of disease (27).
Memantine have no benefit over placebo for those with mild AD (28-29) and thus prescribed in combination with continuing AChEIs treatment. Memantine treatment along with AChEIs treatment provided significant benefit in cognitive and psychiatric symptom compared to the patient receiving a placebo after six month (30). Also combination treatment was found effective to reduce the risk of nursing home admission (31-32).
The only limitation with this medication is that they are only able to provide symptomatic relief and in some cases offer no protection at all. Also the full mechanism behind this medication and the effect they have on the brain are not fully understood. For instance, the effect of AChEIs on cholinergic system is well established but their influence on the brain inflammatory system via nicotinic acetylcholine receptors is only recently becoming appreciated (33). Increase in Antioxidant level with AChEIs treatment (34) and protection from Aß Mediated toxicity (35) have shown by using animal studies. AChEIs treatment has no effect on blood antioxidant (36) or proinflammatory biomarkers levels after one year of treatment (37).
Cardiovascular Risk Factor and Antihypertensive Intervention- The result from large population studies suggest that hypertension (HT) in mild life is a risk factor for late life development of AD (38). Mild hypotension in elderly is associated with lower incidence of AD (39-40) and other type of dementia (41). Panel member of Eight Joint National Committee in 2014, produced report which recommends that hypertension in the elderly (greater than 60 years) is treated with systolic blood pressure = 150 and diastolic blood pressure< 90., as more aggressive treatment to goal SBP>140 and whereas for those over 75 years cardiovascular risk was not affected until SBP>150 Suggesting that cardiovascular risk associated with BP shifts with advancing age (42-43). BPof 135/80 mmHg is associated with best cognitive performance in healthy adults over 65 years. (44)
Antihypertensive Medication- Angiotensin converting enzyme inhibitors (ACEI) and angiotensin receptor 1 blocker are antihypertensive medication which has effect on Renin-Angiotensin system (RAS). AChEIs which penetrate the brain have protective effect on global cognitive test scores in AD patient (45) as compared to non-brain penetrating AChEIs despite successful BP control, leading to suggestion that this medication is able to have influence on cognitive independent of its vasoactive effects. ACEIS and AT1RB increase the level of angiotensin 4 in brain (46-47) and have been found to be effective in improving learning and memory in animal model (48). The exact mechanism behind this are not yet clear, however angiotensin 4 have role in increasing cellular uptake of glucose .
HT and antihypertensive medication may also affect AD associated neuropathology. Level of Aß plaques and NFTs in post mortem brain tissue in AD patient is measured (50). Less plaque in HT patient taking HT medication are observed as compared to patient who did not take HT medication. The effect of HT should not be considered alone in dementia. Several other characteristics are in-volved that include obesity, insulin resistance and low grade chronic inflammation in addition to HT (51). Furthermore no data exist from the study of phase three clinical trials to support the use of antihypertensive medication in management of AD.
Anti-inflammatory Based Intervention- Both peripheral (52-53) and central (54) immune activity is involved in AD patient. Microglia has been observed to be activated by Aß In vitro (55) suggesting inflammation may be triggered by AD pathology. But there is no evidence of positive effect of NSAIDS and other anti-inflammatory treatment and don not appear to be useful as treatment to slow down progression of illness.
Diet- Diet have double edged sword like effect on the development and progression of AD. Diet rich in trans saturated fats, processed sugar and low in poly unsatu-rated fat and other essential nutrients contribute to ill healthy by affecting multiple organs and system.
Obesity has been identified as major risk factor for AD (56-59). The western diet having high level of red meat and saturated fats have been associated with increasing level of AD (60). The Mediterranean diet (MeDi) on other hand has been associated with less risk of AD (61). In early stages of disease, the effect of MeDi diet in slowing progression of AD is investigated by (62). Thus by modifying the diet and control on various factors which indirectly affect the Obesity leads to slowing the progression of AD.
Epigallocatechin -3 gallate and luteolin mainly found in green tea were the two most important mitochondrial restorative compound which decrease the level of MMP (Mitochondrial membrane potential), reactive oxygen species, and ATP level to 50-80 % in mitochondrial isolated from hippocampus, cortex and striatum. The result from the study suggested that Epigallocatechin-3- gallate and luteolin like flavanoids are used as multi-potent therapeutic agent in future. (99)
Various Therapeutic Interventions for Alzheimer which are currently in clinical trials:
Immunotherapy focused on ß amyloid- This include both passive immunization which consist of an injection of pre- prepared antibodies and an active immunization where immune system is stimulated to produce its own antibodies through administration of a vaccine (63).
Prepared and administered antibodies can be precisely directed against APP, monomeric Aß, soluble Aß oli-gomers, insoluble Aß fibrils as well as against Aß carrier protein and transport channels are very important because of our lack of precise knowledge as to which form of Aß Are involved in pathogenesis of AD.
Active Immunization- It involves administration of a vaccine containing an-tigens. This process has both advantages and disad-vantages (63-64). The potential drawback is the diversity of response. The immune system of elderly patient may produce autoimmune system side effect instead of producing appropriate antibodies.
The very first active vaccine against Aß tested in human designated as AN-1792, Contained full length pre-aggregated amyloid peptide (Aß 1-42) (13,65). Be-cause of severe side effect including aseptic menin-goencephalitis in 6% of vaccinated patient with AD (65-66), the phase 2 trial was terminated in January of 2000 (13). Immunological response to vaccine was also weak as compared to placebo-treated control group. In post mortem examination of brain of vaccinated patient, there is decrease level of insoluble amyloid plaques (63). This lead to an important data for further clinical trials. The CAD106 Vaccine contains an Aß1?6 Fragment as potential immunogenic sequence attached to a carrier formed from the coat protein of bacteriophage Qß as an adjuvant (13). It did not lead to adverse effect observed in case of AN-1792 in phase 2 trial and 75% of patient responded with antibody production in adequate level (67). But the study did not confirm clinical efficacy in term of difference between treated group and control group. Phase 2 trials results are yet to be published done in December 2012 (68). The next vaccine designated as ACC-001 Contain six amino acid sequences Aß
Passive Immunization- It is most widely developed approach in clinical trials in which the administered antibodies are exogenous and are delivered from a source other than patient’s own immune system. They are usually including humanized murine monoclonal antibody or donor- derived human polyclonal antibodies. The advantage of this approach is rapid clearance of antibody in case of side effects because of adminis-tration of known amount of specific antibody.
The first humanized monoclonal antibody was Bapineuzumab used against the Aß N- Terminus Aß1-5 which binds more strongly to deposit amyloid plaques than to soluble Aß monomer. Bapineuzumab advances to next phase although the result of phase 2 trial were not unequivocal but in phase 3 trials, double bind placebo controlled parallel group did not confirm drug’s efficacy while showing its adverse effect (13,68) which include vasogenic edema and intracerebral microhemorrhage detected by magnetic resonance imaging as amyloid related imaging abnormalities(ARIA).
Better outcomes were seen in case of solanezumab, a humanized monoclonal antibody. It is specific to the mid domain of the Aß peptide (Aß16-24) and binds selectively to monomeric soluble toxic species of Aß. Phase 3 trials involving over 2000 patient from 16 countries with, mild to moderate AD revealed reduction in cognitive decline by 34% but only for patient with mild type of disease (13,66,70).
Gantenerumab is conformational antibody and is able to specifically bind to aggregated Aß In the brain. It possess two binding sited, one which interfere with N- terminus of region of Aß While other binds to the mid domain of Aß peptide (14). Currently Gantenerumab is in phase 2/3 trials and last until 2016.
Genezumab is novel human IgG4 monoclonal antibody which binds to Aß oligomers fibrils and plaques and inhibiting its aggregation and promoting disaggregation. Currently it is in phase 2 trial with mild to moderate AD patient. (14)
Intravenous Immunoglobulin (IVIG)- It is the mixture of polyclonal antibodies prepared from blood plasma of thousands of healthy young volunteers (63). IVIG has strong affinity for neurotoxic oligomers and Aß Fibrils and display potent immune modulating and inflammatory effect. But lack of positive result in phase 3 trial conducted in nov 2012 in US resulted in termination of study (14,68).
Decreasing Aß Production-Secretase Inhibitors- It generally includes two classes.
y - SecretaseInhibitors and modulators- Role of ß and y Secretase is considered as target in search for new AD treatment strategy because of role in formation of various aggregate of amyloid protein (71). This enzyme is composed of Presenilin 1, Nicastrin, Anterior pharynx defective-1(APH-1) and Presenilin 1 enhancer-2 (PEN-2) (72).y- Secretase complex is involved in proteolysis of more than 90 other intramembranous signaling proteins (73).
Semagacestat is the first drug which is non-selective y- Secretase inhibitors and failed in two large phase 3 studies with more than 2600 patient from 31 countries (72,74). The reason behind failure of non-selective inhibitors was because of omnidirectional role of Presenilin1, a catalytic subunit ofy- Secretase (75) The most important adverse effect associated with y- Secretase include hematological dis-orders, gastrointestinal symptom, skin reaction and hair color change (76). These entiresymptom are mainly caused by impaired Notch Transduction due to complete inhibition of the enzyme.
Second generation y- Secretase inhibitors avoid influ-ence on Notch protein Transformation result in im-proving their safety profile (77). The first y-Secretase modulator to undergo clinical trial was Avagacestat (BMS-708163) (68). Other y- Secretase modulator that is Begacestat (GSI-953) stopped in phase 1 trial.
ß - Secretase Inhibitors- Another target interfering with amyloid formation pathway is ß Secretase which belong to group of as-partyl proteases. Apart from involvement in amyloi-dogenic metabolism of APP, it play important role in metabolism of other protein including neuregulin 1(NGR 1) responsible for myelination of neuron (78).
The most promising inhibitor is MK-8931 which successfully passed safety profile involving 88 healthy volunteer in 2012 (68). Phase 1b study in 32 patients confirmed the safety and efficacy of MK-8931(79). Phase 2/3 trial with 2000 and 1500 patient is currently underway (68).
Another ß- Secretase inhibitor LY2886721 Passed phase 1 trial but phase 2 studies with 130 patients exhibiting mild AD was disemtinued in June 2013 due to abnormal liver biochemical test (79-80).
Immunotherapy Directed Against Tau protein- Recent Research has shown that the antibodies against pathological tau protein which are able to cross blood brain barrier are transferred into neuron with participation of Fc receptor and via endosemal/liposomal system, it bind to pathological tau protein (81). AADvac 1 is the first vaccine and is currently undergoing phase 1 clinical trial.
Blocking Phosphorylation of tau protein- Protein kinases are class of enzymes involved in tau phosphorylation and most important of them is glycogen synthase kinase 3 beta (GSK-3ß) and has been reported that neurotoxic Aß promotes GSK-3ß activity thus GSK-3ß inhibitors are potent drug targets.
Tideglusib (NPO31112, NP-12) is an irreversible GSK-3ß inhibitor and shown to reverse amyloid load in brain tissue, prevent cell loss and reduce spatial memory deficit in preclinical studies (1,69). In preliminary study patient exhibited slightly improved cognitive function measured using Mini Mental State Examination and cognitive scales in mild to moderate AD cases (82-83).
Intranasal insulin may decrease the activity of GSK-3ß And lead to inhibition of tau phosphorylation thus have role in treatment of AD (84). Phase 3 clinical trial are currently undergoing for Humulin R in patient with mild type of AD.
Other mechanism- Serotonin is a neurotransmitter which indirectly affects the neurodegenerative process. 5-HT6 Serotonin receptors present in brain are mainly responsible for memory and cognitive function (85). Blocking of 5HT6 Receptors result in increased level of acetylcholine in synaptic cleft lead to improve in cholinergic transmis-sion and hence enhancing memory and cognitive functions. It is known that cholinergic activity generally deteriorates due to degeneration of cholinergic neurons in case of Alzheimer disease. Therefore the compound which affects the 5HT6 Receptors are po-tential therapeutic targets for symptomatic treatment of AD. (86)
Idalopirdine (Lu AE58054) is a selective 5HT6receptor antagonist which successfully passed a phase 1 study in healthy volunteers exhibiting good safety profile (87-88).From the result of preclinical studies, it has been suggested that the use of 5HT6 antagonist along with cholinesterase inhibitor may increase beneficial effect on cognition. (89). Phase 2 study was carried out among 278 patient out of which 133 received placebo and 145 received the drug with mild form of AD, taking donepezil 10 mg daily for at least four month (87,90) indicate improvement in cognitive function measured using ADAS-cog subscale with few side effects.
Histamine H3 receptor antagonists- Histamine H3 receptors both auto and heteroreceptors are present in large amount in structure of brain-mainly prefrontal cortex, hippocampus and hypothalamus and are responsible for memory and cognitive processes (91). The H3 receptor is a presynaptic receptor and blocking of which leads to increase release of acetylcholine, dopamine, GABA, noradrenaline and histamine in synaptic cleft. H3 receptor antagonist may indirectly improve cholinergic neurotransmission (92). ABT-288 is a competitive selective H3 receptor antagonist which demonstrated a good safety profile and tolerability in phase 1 studies involving healthy volunteers (93-94) and recently completed phase 2 clinical trial involving 242 patients with mild to moderate AD (95).GSK239512 is another H3 antagonist which is also currently undergoing phase 2 trial on patient with mild to moderate AD (NCT01009255) (68,96).
Enhancement of acetylcholine response of a-7 nicotinic acetylcholine receptors- Encenicline (EVP-6124, MT-4666) is partial a-7 nico-tinic acetylcholine receptor selective agonist which has been evaluated for treatment of AD and cognitive deficits in Schizophrenia. It act as co agonist with ace-tylcholine and being selective a7-nAChR agonist may enhance cognition without causing side effects relating to over activation of other nAChR subunits or muscarinic acetylcholine receptors(97). Phase 2 trial have confirmed the positive result of drug safety and efficacy by the ADS-cog-13 subscale.
SUMMARY- Interesting Therapeutic approaches including NMDA receptor antagonism, modulation of calcium homeos-tasis, reducing the oxidative stress that is antioxidant effect, statin therapy and potential therapeutic approaches which mainly target on anti Aß agents such as vaccines, antibodies and inhibitors and modulators of ? and ß Secretase, agent blocking the phosphorylation of tau protein as well as agent which affect the neurotransmitter release (like serotonergic 5HT6 and histaminergic H3. It is known that development of newtherapeutic agent is very time consuming and complex process with 95% chances of failure. Most of the drug which passes the phase 2 trial studies generally fails in phase 3 trial because of the lack of therapeutic potential, some serious adverse effects and unknown drug safety profile. Number of drugs is currently under clinical trial studies but none of them are approved for use in AD treatment thus this article presents the future direction for seeking novel, safe and effective treatment for AD.
REFERENCES:
- Anand R, Gill KD, Mahdi AA. Therapeutics of Alzheimer’s disease: past, present and future. Neuropharmacology 2014; 76(Part A):27–50.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet 2005; 366(9503):21127.
- Wimo A, Jonsson L, Bond J, Prince M, Winblad B. Alzheimer Disease international. The worldwide economic impact of dementia 2010.Alzheimers Dement 2013;9(1): 1–11.
- McKhann, G.M et al., 2011. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement, 7: 263-269.
- Justyna Godyn, jakub jonczyk, et. al., 2015. Therapeutic strategies for Alzheimer’s disease in Clinical trials. Pharmacological Reports 68(2016):127-138.
- Giannakopoulos, P. et al., 2003. Tangle and neuron numbers but not amyloid load, predict cognitive status in Alzheimer’s disease. Neurology, 60:1495-1500.
- Aizenstein, H.J. et al., 2008.Frequent amyloid deposition without significant cognitive impairment among elderly. ArchNeurol, 65:1509-1517.
- Davies P, Maloney AJ. Selective loss of central cholinergic neurons in Alzheimer’s disease. Lancet 1976; 2 (8000):1403.
- M.H. Eskelinen, T. Ngandu, E.L. Helkala, J. Tuomilehto, A. Nissinen, H. Soininen, M.Kivipelto, Fat intake at midlife and cognitive impairment later in life:a population-based CAIDE study, International Journalof Geriatric Psychiatry 23 (7)(2008) 741–747.
- G.M. Pasinetti, J.A. Eberstein, Metabolic syndrome and the role of dietary lifestylesin Alzheimer's disease, J. Neurochem. 106 (4) (2008) 1503–1514.
- G. Winocur, C.E. Greenwood, G.G. Piroli, C.A. Grillo, L.R. Reznikov, L.P. Reagan, B.S.McEwen, Memory impairment in obese Zucker rats: an investigation of cognitivefunction in an animal model of insulin resistance and obesity, Behav. Neurosci, 119 (5) (2005) 1389.
- Lundkvist J, Halldin MM, Sandin J, Nordvall G, Forsell P, Svensson S, et al. The battle of Alzheimer’s disease – the beginning of the future unleashing the potential of academic discoveries. Front Pharmacol 2014; 5: 102.
- Wisniewski T, Goni F. Immunotherapy for Alzheimer’s disease. Biochem Pharmacol 2014; 88(4):499–507.
- Jia Q, Deng Y, Qing H. Potential therapeutic strategies for Alzheimer’s disease Targeting or beyond beta-amyloid: insights from clinical trials. BiomedResInt 2014; 2014:837157.
- Kumar A, Singh A. Ekavali. A review on Alzheimer’s disease pathophysiology and its management: an update. Phar-macol Rep, 2015; 67(2):195–203.
- Klinkenberg, I., Sambeth et al., 2011.Acetylcholine and attention.BehavBrainRes, 221:430-442.
- Auld, D.S. et al., 2002. Alzheimer’s disease and the basal forebrain cholinergic system: relation to beta amyloid peptides, cognition and treatment strategies. Prog Neurobiol, 68:209-245.
- Danysz, W and Parsons, 2012.Alzheimer’s disease, ß-amyloid, glutamate, NMDA receptors and Memantine searching for the connections. Br J Pharmacol, 167:324-352.
- Rogers, S.L., 1998. Prespectives in the management of Alzheimer disease: clinical profile of donepezil. Dementiaandgeriatriccognitivedisorders, 9 suppl 3:29-42.
- Rogers, S.L and Friedhoff, L.T., The efficacy and safety of donepezil in patient with Alzheimer disease: results of a US Multicentre, Randomized, Double-Blind, Placebo- controlled Trial. The Donepezil study group.Dementia (Basel, Switzerland), 7(6):293-303.
- Sabbagh, M. et al., 2013. Evaluating the cognitive effects of donepezil 23 mg/d in moderate and severe Alzheimer’s disease: analysis of effects of baseline features on treatment response. BMC Geriatrics, 13:56
- Small, G.W. et al., 2005. Cognitive performance in Alzheimer’s disease patients receiving rivastigmine for up to 5 years. International journal of clinical practice, 59(4): 473–7.
- Winblad, B. et al., 2007.A six-month double-blind, randomized, placebo-controlled study of a transdermal patch in Alzheimer’s disease--rivastigmine patch versus capsule. Internationaljournal of geriatric psychiatry, 22(5):456–67.
- Seibert, J. et al., 2012.Effectiveness and tolerability of transdermal rivastigmine in the treatment of Alzheimer’s disease in daily practice. Neuropsychiatric Disease and Treatment, 8:141–7.
- Articus, K. et al., 2011. A 24-week, multicenter, opens evaluation of the clinical effectiveness of the rivastigmine patch in patients with probable Alzheimer’s disease. International journal of clinical practice, 65(7):790–6.
- Wilkinson, D. and Murray, J., 2001. Galantamine: a randomized, double-blind, dose comparison in patients with Alzheimer’s disease. International journal of geriatric psychiatry, 16(9):852–7.
- Gillette-Guyonnet, S. et al., 2011.Long-term progression of Alzheimer’s disease in patients under antidementia drugs.Alzheimer’s and dementia: the journal of the Alzheimer's Association, 7(6):579–92.
- Schmeidler, J., Mohs, R.C. and Aryan, M., 1998. Relationship of disease severity to decline on specific cognitive and functional measures in Alzheimer disease.Alzheimer Dis Assoc Disord, 12:146–151.
- Schneider, L.S. et al., 2014. Clinical trials and late-stage drug development for Alzheimer’s disease: an appraisal from 1984 to 2014. J Intern Med, 275:251–283.
- Tariot, P.N. et al., 2004. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA, 291(3): 317–24.
- Lopez, O.L. et al., 2009.Long-term effects of the concomitant use of Memantine with cholinesterase inhibition in Alzheimer disease.Journal of neurology, neurosurgery, and psychiatry, 80(6):600–7.
- 32 Lopez, O.L. et al., 2013.The long-term effects of conventional and atypical antipsychotics in patients with probable Alzheimer’s disease. The American journal of psychiatry, 170(9):1051–8.
- Tabet, N., 2006. Acetyl cholinesterase inhibitors for Alzheimer’s disease: anti-inflammatories in acetylcholine clothing! Age Ageing, 35:336–338.
- Zhang, H.Y. and Tang, X.C., 2000. Huperzine B, a novel acetyl cholinesterase inhibitor, attenuates hydrogen peroxide induced injury in PC12 cells. Neurosci Lett, 292:41–44.
- Kimura, M. et al., 2005.Protective effect of donepezil against Abeta (1-40) neurotoxicity in rat septal neurons. Brain Res, 1047:72–84.
- Klugman, A. et al., 2012. Antioxidant enzymatic activities in Alzheimer’s disease: the relationship to acetyl cholinesterase inhibitors. J Alzheimers Dis, 30:467–474.
- Richardson, C. et al., 2013.Blood pro-inflammatory cytokines in Alzheimer’s disease in relation to the use of acetylcholinesterase inhibitors.Int J Geriatr Psychiatry, 28, pp.1312–1317.
- Qiu, C. et al., 2003. Low blood pressure and risk of dementia in the Kungsholmen project: a 6-year follow-up study. Archives of neurology, 60(2):223–8.
- Guo, Z. et al., 1999. Low blood pressure and incidence of dementia in a very old sample: dependent on initial cognition. J Am Geriatr Soc, 47:723–726.
- Kokmen, E. et al., 1991. Clinical risk factors for Alzheimer’s disease: a population-based case control study. Neurology, 41:1393–1397.
- Petitti, D.B. et al., 2005. Blood pressure levels before dementia. Arch Neurol, 62:112–116.
- James, P.A. et al., 2014. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA: the journal of the American Medical Association, 311(5):507–20.
- Ogihara, T. et al., 2008. The optimal target blood pressure for antihypertensive treatment in Japanese elderly patients with high-risk hypertension: a subanalysis of the Candesartan Antihypertensive Survival Evaluation in Japan (CASE-J) trial. Hypertension research: officialjournal of the Japanese Society of Hypertension, 31(8):1595–601.
- Liu, H. et al., 2013. Optimal blood pressure for cognitive function: findings from an elderly African- American cohort study. Journal of the American Geriatrics Society, 61(6):875–81.
- Ohrui, T. et al., 2004.Effects of brain-penetrating ACE inhibitors on Alzheimer disease progression. Neurology, 63:1324–1325.
- Fournier, A. et al., 2009. Prevention of dementia by antihypertensive drugs: how AT1-receptorblockers and dihydropyridines better prevent dementia in hypertensive patients than thiazides and ACE-inhibitors. Expert review of neurotherapeutics, 9(9):1413–31.
- Gard, P.R. and Rusted, J.M., 2004. Angiotensin and Alzheimer’s disease: therapeutic prospects. Expert Rev Neurother, 4:87–96.
- Paris, J.J. et al., 2013. Central administration of angiotensin IV rapidly enhances novel object recognition among mice. Neuropharmacology, 70:247–253.
- Vanderheyden, P.M., 2009. From angiotensin IV binding site to AT4 receptor. Mol Cell Endocrinol, 302:159–166.
- Hoffman, L.B. et al., 2009.Less Alzheimer disease neuropathology in medicated hypertensive than non-hypertensive persons. Neurology, 72(20):1720–6.
- Misiak, B., Leszek, J. and Kiejna, A., 2012. Metabolic syndrome, mild cognitive impairment and Alzheimer’s disease--the emerging role of systemic low-grade inflammation and adiposity. Brain Res Bull, 89:144–149.
- Maes, M. et al., 1999.Inflammatory markers in younger vs elderly normal volunteers and in patients with Alzheimer’s disease. J Psychiatr Res, 33:397–405.
- Remarque, E.J. et al., 2001. Patients with Alzheimer’s disease display a pro-inflammatory phenotype. Exp Gerontol, 36:171–176.
- Webster, S., Bonnell, B. and Rogers, J., 1997.Charge-based binding of complement component C1q to the Alzheimer amyloid beta-peptide. Am J Pathol, 150:1531-1536.
- Maezawa, I. et al., 2011. Amyloid-beta protein oligomer at low nanomolar concentrations activates microglia and induces microglial neurotoxicity. The Journal of biological chemistry, 286(5):3693–706.
- Hassing, L.B. et al., 2004. Comorbid type 2 diabetes mellitus and hypertension exacerbates cognitive decline: evidence from a longitudinal study. Age Ageing, 33:355–361.
- 57 Kivipelto, M. et al., 2001. Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ, 322:1447–1451.
- Whitmer, R.A. et al., 2007.Body mass index in midlife and risk of Alzheimer disease and vascular dementia. Current Alzheimer research, 4(2):103–9.
- Luchsinger, J.A., 2010. Type 2 diabetes, related conditions, in relation and dementia: an opportunity for prevention? Journal of Alzheimer’s disease: JAD, 20(3):723–36.
- Grant, W.B., 2014. Trends in diet and Alzheimer’s disease during the nutrition transition in Japan and developing countries. Journal of Alzheimer’s disease: JAD, 38(3): 611–20.
- Scarmeas, N. et al., 2007.Mediterranean diet and Alzheimer disease mortality. Neurology, 69(11):1084–93.
- Frisardi, V. et al., 2010. Nutraceutical properties of Mediterranean diet and cognitive decline: possible underlying mechanisms. Journal of Alzheimer’s disease: JAD, 22(3):715–40.
- Lannfelt L, Relkin NR, Siemers ER. Amyloid-ss-directed immunotherapy for Alzheimer’s disease. J Intern Med 2014; 275(3):284–95.
- Paquet C, Amin J, Mouton-Liger F, Nasser M, Love S, Gray F, et al. Effect of active Abeta immunotherapy on neurons in human Alzheimer’s disease. JPathol 2015;235(5):721–30.
- Panza F, Logroscino G, Imbimbo BP, Solfrizzi V. Is there still any hope for amyloid-based immunotherapy for Alzheimer’s disease? Curr Opin Psychiatry 2014; 27(2):128–37.
- Panza F, Solfrizzi V, Imbimbo BP, Tortelli R, Santamato A, Logroscino G. Amy- loid-based immunotherapy for Alzheimer’s disease in the time of prevention trials: the way forward. Expert Rev Clin Immunol 2014; 10(3):405–19.
- Winblad B, Andreasen N, Minthon L, Floesser A, Imbert G, Dumortier T, et al. Safety, tolerability, and antibody response of active Abeta immunotherapy with CAD106 in patients with Alzheimer’s disease: randomised, double-blind, placebo- controlled, first-in-human study. Lancet Neurol 2012; 11(7):597–604.
- https://clinicaltrials.gov.
- Arai H, Suzuki H, Yoshiyama T, Lobello K, Peng Y, Liu E, et al. Safety, tolerability and immunogenicity of an immunotherapeutic vaccine (vanutide cridificar [ACC-001]) and the QS-21 adjuvant in Japanese individuals with mild-to-moderate Alzheimer’s disease: a phase IIa, multicenter, randomized, adjuvant and placebo clinical trial. Alzheimer’sDement 2013;9(4):282.
- Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, et al. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s disease. N Engl J Med 4; 370(4):311–21.
- Golde TE, Koo EH, Felsenstein KM, Osborne BA, Miele L. gamma-Secretase inhibitors and modulators. Biochim Biophys Acta 2013;1828(12):2898–907.
- Mikulca JA, Nguyen V, Gajdosik DA, Teklu SG, Giunta EA, Lessa EA, et al. Potential novel targets for Alzheimer pharmacotherapy: II. Update on secretase inhibitors and related approaches. J Clin Pharm Ther 2014; 39 (1):25–37.
- Haapasalo A, Kovacs DM.The many substrates of presenilin/ gamma-secretase. J Alzheimers Dis 2011; 25 (1):3–28.
- Roher AE, Maarouf CL, Kokjohn TA, Whiteside CM, Kalback WM, Serrano G, et al. Neuropathological and biochemical assessments of an Alzheimer’s disease patient treated with the gamma-secretase inhibitor semagacestat. Am J Neurodegener Dis 2014; 3(3):115–33.
- Artavanis-Tsakonas S, Rand MD, Lake RJ. Notch signaling: cell fate control and signal integration in development. Science 1999; 284(5415):770–6.
- Hsu CK, Hsu CC, Lee JY, Kuo YM, Pai MC. Exacerbation of psoriatic skin lesions in a patient with Alzheimer disease receiving gamma-secretase inhibitor. J Am Acad Dermatol 2013; 68(2):e46–8.
- Imbimbo BP. Therapeutic potential of gamma-secretase inhibitors and modulators. Curr Top Med Chem 2008; 8(1): 54–61.
- Willem M, Garratt AN, Novak B, Citron M, Kaufmann S, Rittger A, et al. Control of peripheral nerve myelination by the beta-secretase BACE1. Science 2006; 314(5799):664–6.
- Yan R, Vassar R. Targeting the beta secretase BACE1 for Alzheimer’s disease therapy. Lancet Neurol 2014; 13(3):319–29.
- Lahiri DK, Maloney B, Long JM, Greig NH. Lessons from a BACE1 inhibitor trial: off-site but not off base. Alzheimers Dement 2014; 10(5 SUPPL):S411–9.
- Novak M. Tau vaccine: active immunization with misfolded tau protein attenuates tau pathology in the transgenic rat model of tauopathy. Alzheimer’s Dement 2009; 5(4):93.
- Del Ser T, Steinwachs KC, Gertz HJ, Andres MV, Gomez-Carrillo B, Medina M, et al. Treatment of Alzheimer’s disease with the GSK-3 inhibitor tideglusib: a pilot study. J Alzheimers Dis 2013; 33(1):205–15.
- Sereno L, Coma M, Rodriguez M, Sanchez-Ferrer P, Sanchez MB, Gich I, et al. A novel GSK-3beta inhibitor reduces Alzheimer’s pathology and rescues neuronal loss in vivo. Neurobiol Dis 2009; 35(3):359–67.
- Yang Y, Ma D, Wang Y, Jiang T, Hu S, Zhang M, et al. Intranasal insulin ameliorates tau hyperphosphorylation in a rat model of type 2 diabetes. J Alzheimers Dis 2013;33(2):329–38.
- Marcos B, Cabero M, Solas M, Aisa B, Ramirez MJ. Signaling pathways associated with 5-HT6 receptors: relevance for cognitive effects. Int J Neuropsycho pharmacol 2010; 13(6):775–84.
- Marazziti D, Rutigliano G, Catena-DelL’Osso M, Baroni S, Dell’Osso L. The 5- HT6 receptor antagonism approach in Alzheimer’s disease. Drugs Future 2014; 39(2):133–40.
- Wilkinson D, Windfeld K, Colding-Jorgensen E. Safety and efficacy of idalopirdine, a 5-HT6 receptor antagonist, in patients with moderate Alzheimer’s disease (LADDER): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol 2014; 13(11):1092–9.
- Schneider LS. Idalopirdine for Alzheimer’s disease: written in the stars. Lancet Neurol 2014; 13(11):1063–5.
- Marcos B, Chuang TT, Gil-Bea FJ, Ramirez MJ. Effects of 5-HT6 receptor antagonism and cholinesterase inhibition in models of cognitive impairment in the rat. Br J Pharmacol 2008; 155(3):434–40.
- Wilkinson D, Colding-Jorgensen E, Windfeld K. A clinical phase II study of LU AE58054 added to stable donepezil treatment in patients with moderate Alzheimer’s disease. Alzheimer’s Dement 2013; 9(4):529.
- Motawaj M, Burban A, Davenas E, Gbahou F, Faucard R, Morisset S, et al. The histaminergic system: a target for innovative treatments of cognitive deficits. Therapie 2010; 65(5):415–22.
- Esbenshade TA, Browman KE, Bitner RS, Strakhova M, Cowart MD, Brioni JD. The histamine H3 receptor: an attractive target for the treatment of cognitive disorders. Br J Pharmacol 2008; 154(6):1166–81.
- Esbenshade TA, Browman KE, Miller TR, Krueger KM, Komater-Roderwald V, Zhang M, et al. Pharmacological properties and procognitive effects of ABT- 288, a potent and selective histamine H3 receptor antagonist. J Pharmacol ExpTher 2012; 343 (1):233–45.
- Othman AA, Haig G, Florian H, Locke C, Gertsik L, Dutta S. The H3 antagonist ABT-288 is tolerated at significantly higher exposures in subjects with schizophrenia than in healthy volunteers. Br J Clin Pharmacol 2014; 77 (6): 965–74.
- Haig GM, Pritchett Y, Meier A, Othman AA, Hall C, Gault LM, et al. A randomized study of H3 antagonist ABT-288 in mild-to-moderate Alzheimer’s dementia. J Alzheimers Dis 2014; 42(3):959–71.
- Grove RA, Harrington CM, Mahler A, Beresford I, Maruff P, Lowy MT, et al. A randomized, double-blind, placebo-controlled, 16-week study of the H3 receptor antagonist, GSK239512 as a monotherapy in subjects with mild-to-moderate Alzheimer’s disease. Curr Alzheimer Res 2014; 11(1): 47–58.
- Prickaerts J, van Goethem NP, Chesworth R, Shapiro G, Boess FG, Methfessel C, et al. EVP-6124, a novel and selective alpha7 nicotinic acetylcholine receptor partial agonist, improves memory performance by potentiating the acetylcholine response of alpha7 nicotinic acetylcholine receptors. Neuropharmacology2012; (2):1099–110.
- Trevor J Crawford, Steve Higham, Distinguishing between impairment of working memory and inhibitory control in case of early dementia. Neuropsychologia, 81 (2016) 61-67.
- Draqicevic N, Smith A, Lin X, Green tea eppigallocatechin- 3- gallate and other flavanoids reduce Alzheimer amyloid induced mitochondrial dysfunction. J Alzheimer Dis. 2011; 26(3).
| Source of Financial Support: Nil Conflict of interest: Nil |