ABSTRACT- Introduction: Blood group antigens have been reported to be associated with many diseased conditions severally. Studies have suggested that ABO blood groups have an impact on infection status of the individuals possessing a particular blood group due to the significant associations observed when analyzed. However there is limited information on the relationship between these blood group antigens with haemoglobin genotype and CD4 cell count in Human Immunodeficiency Virus (HIV) infection, hence the need for this study.
Materials and Method: Exactly 240 newly enrolled seropositive patients attending the HIV Clinic of LAUTECH Teaching Hospital, Osogbo, Nigeria and 120 healthy blood donors were recruited for this study. Antibodies to HIV were determined using determine rapid HIV 1/HIV 2 test kit (Abbott), enzyme linked immunosorbent assay (ELISA) (GenScreen plus HIV Ag-Ab test kit, Paris) and Western blot (New-LAV Blot 1, BioRad, France) for confirmatory test. ABO and Rhesus blood grouping was determined by standard tile and tube techniques. Haemoglobin genotype determined by alkaline cellulose acetate haemoglobin electrophoresis while CD4 cell count was estimated with Partec Cyflow analyser.
Result: There is no significant association between the ABO/Rh antigens and haemoglobin genotypes of the test and control groups (P<0.05). All participants in the control group had CD4 count >200cells/mm3 while 198 (55%) HIV infected subjects had CD4 count >200cells/mm3 and 42 (11.7%) had CD4 count <200cells/mm3. A significant association was observed between the CD4 cell count of the patients and their ABO blood group antigens (P<0.05) with blood group A and AB having the highest CD4count.
Conclusion: The outcome of this study reiterates the fact that blood group antigens are involved in immune protection against infectious disease. Blood group A which has been implicated to confer susceptibility in some diseased condition has been observed to confer immunity in this study.
Key-words- CD4 cells, Blood Group Antigens, HIV and Haemoglobin Genotype
INTRODUCTION
Blood group antigens have been reported severally to be associated with many disease conditions [1-2]. Studies have suggested that ABO blood groups have an impact on immunity to infection in individuals possessing a particular blood group due to the significant associations observed when investigated [3-6].
The ABO blood group system which was first discovered by Landsteiner in 1901[7-9] is therefore one of the series ofglycoproteins and glycolipids present on the human red cell which constitute the red cell antigen. The Rh was later discovered by Landsteiner and Weiner in 1941[10]. These antigens which are genetically controlled, are inherited in Mendelian fashion, appear early in life and remain unchanged till death [7]. About 700 erythrocyte antigens have been described and organized into 30 blood group systems by the International Society of Blood Transfusion out of which ABO and Rh are the most important [8].
Blood group antigens plays a vital role in transfusion safety, understanding genetics, inheritance pattern, researching population migration patterns, as well as resolving certain medico-legal issues [11]. In modern medicine besides their importance in evolution, their relation to disease and environment is being increasingly important. Some blood groups can act as a receptor and ligand for bacteria, parasites and viruses. The possible pathogenesis for this susceptibility is that as many organisms that may bind to polysaccharide on cells and soluble blood group antigens may block this binding [12-13].
Pathologically, certain blood groups have been associated with diseases. For example, blood group A individuals are known to be more susceptible to coronary heart disease (CHD) independent of known risk factors than other ABO blood groups [14]. Also these same groups A individuals have higher levels of low density lipoprotein (LDL) cholesterol [15]. Although the molecular aspects of this observation still remain to be elucidated, the observation implies that, this antigen has potential to either influence synthesis or inhibit the natural metabolism of these lipids, thus, predisposing individuals to CHD while group O individuals were reported to have a lower risk for this condition. In addition, blood group A and B are known to be highly susceptible to thrombotic disorders in contrast to group O individuals who are more at risk for bleeding than thrombotic events [17-19].
Blood group A individuals have also been associated with malignancies such as cancer of the ovary, cervix, rectum, breast, and stomach and leukemia [15-16]. This is thought to be due to an abundance of high-affinity binding sites for epidermal growth factor (EGF) on blood group A red blood cells compared to blood groups O and B [20]. Since blood groups may be expressed on tissues other than red cells, it is likely that the binding of EGF to these binding sites may indeed promote cancer development. Gastric carcinomas were found to be associated with increased expression of ABH and Lea antigens while colonic cancers were associated with expression of Leb and low expression of the other antigens [21].
Several studies have also investigated the association of blood groups with infectious and non-infectious diseases. Among infectious disease, Human immunodeficiency virus (HIV), and Hepatitis virus are of great concern because of their prolonged viraemia as well as carrier or latent state. These infections also cause fatal, chronic and life-threatening disorders [22].
AIDS pandemic in Africa has become in the space of 20 years a real development problem for almost all countries in this continent because it affects the most active age group of the population (15-49 years). HIV continues to be a major public health problem with over 34 million deaths up till 2012 [23]. In 2014, about 1.2 million people died of HIV-related causes in the world, sub-Saharan Africa is the most affected region with almost 70% of new infections. In 2012, the prevalence of HIV in Nigeria was projected to be 3.27% of the general population which was a drop from 3.34% of 2011 [24].
CD4+ cell counts have been studied severally as markers of the progression of HIV infection [25-27], discovered as a measure of the relative risk of developing opportunistic infections [28], function to estimate the impact of HIV and the use of antiretroviral drugs on the epidemiological progression of tuberculosis (TB) [29]. Also CD4+can be used to estimate the proportion of malaria that is attributable to HIV in sub-Saharan Africa [30] and its depletion has also been observed to have a direct correlation with pulmonary tuberculosis in HIV patients [31]. CD4+ cells orchestrate the immune response to attack by HIV, but HIV invades CD4+ cells and uses them to replicate itself. Soon after infection with HIV, CD4+ cells counts decrease by approximately one-quarter and then decrease slowly thereafter [29].
Considering the paucity of information on the distribution of the blood group antigens, haemoglobin genotype and their relationship with the CD4 T cells in HIV infected patients especially in this region, this study therefore aims at providing more information on this subject.
MATERIALS AND METHODS
Subject selection and Sample collection-
A total of 360 subjects aged >16 years, made up of 240 newly enrolled HIV seropositive patients, who are 153 females and 87 males, attending the HIV Reference Clinic of LAUTECH Teaching Hospital, Osogbo, Nigeria and 120 apparently healthy blood donors were recruited for this study.
About 5 ml of venous blood was collected into ethylene diamine tetra acetic acid (EDTA) bottle and plain bottle for HIV testing, ABO and Rhesus blood grouping. Antibodies to HIV were determined using Determine rapid HIV 1/HIV 2 test kit (Abbott), enzyme linked immunosorbent assay (ELISA) (GenScreen plus HIV Ag-Ab test kit, Paris) and Western blot (New-LAV Blot 1, BioRad, France) for confirmatory test. ABO and Rhesus blood grouping was determined by standard tile and tube techniques using standard Anti- A, Anti- B and anti-D reagents (Rapid Labs Ltd, UK). Haemoglobin genotype was determined by alkaline cellulose acetate haemoglobin electrophoresis while CD4 cell count was estimated with Partec Cyflow analyzer.
Informed consent was obtained from the participants. Ethical approval was also obtained from the Ethical committee of Ladoke Akintola University of Technology Teaching Hospital, Osogbo, Nigeria.
STATISTICAL ANALYSIS
Statistical package for Social Science software (SPSS Version 20) was used in the study. Frequency distributions were performed; non-parametric Chi-square and T- independent test was used to test the association between variables. P<0.05 was considered to be statistically significant.
RESULTS
The 240 HIV infected patients consisted of 153 male and 87 female patients, who was newly enrolled and not yet placed on antiretroviral therapy (ART)) while the 120 control subjects are made up of 80 male and 40 female subjects. The result obtained in this study is represented in Table 1 with 132 (36.7%), 54(15.5%), 45(12.5%), 9(2.5%) and 70(19.4%), 25(6.9%), 20(5.6%) and 5(1.4%) being blood group O,A,B and AB respectively in the HIV infected patients and control groups showing no significant association between the two groups (P>0.05). Also 204(56.7%), 100(27.8%) are Rhesus D positive,
while 36(10%), 20(5.6%) are Rhesus D Negative in the subject and control groups respectively. The haemoglobin genotype reveals haemoglobin AA has the highest population frequency when compared with Hb AS and Hb AC respectively.
There is a significant association in the CD4 cell count between the study group and the control group with 198 (55%) subject having normal CD4 cell count (>200cells/mm3) and 42 (11.7%) with low (<200cells/mm3) CD4 count respectively while the entire control subject had normal CD4 count (Table 1). It was observed in Table 2 that there is a significant association between ABO blood groups and CD4 level, Haemoglobin genotype and CD4 level.
Table 1: Frequency Distribution of the Blood groups, Haemoglobin genotypes and the CD4 cell count
| SUBJECT | CONTROL | X2 | P value | |
|---|---|---|---|---|
| ABO Blood Group | ||||
| |
||||
| | ||||
| | ||||
| | ||||
| Hb Genotype | ||||
| CD4 (cells/mm3) | ||||
| | ||||
Table 2: Mean+SD of CD4 cell count and ABO/Rh Blood groups, Haemoglobin Pattern of the HIV infected patients
| ABO Blood Group | F value | P value | ||||
|---|---|---|---|---|---|---|
| A | AB | B | O | |||
| Rh Blood Group | ||||||
| Haemoglobin Electrophoretic Pattern | ||||||
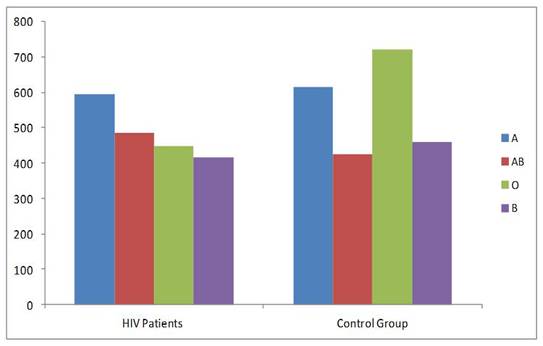
The association between the ABO blood group and CD4 cell count is represented in Fig. 1 displaying blood groups A and AB population has the highest CD4 cell count while blood group O and B population has the lowest CD4 count.
DISCUSSION
Association of the ABO and Rh blood group system with diverse diseased conditions has been established severally through different studies [3-6, 22]. This study also provides more information on the association between ABO/Rh blood group system, haemoglobin electrophoretic pattern and CD4 cell distribution in HIV infection.
In this study the ABO and Rh D blood group system patterns are not significantly associated with HIV infected subjects with the blood groups distributed in the order blood group O, A, B and AB while Rh D positive population larger than the Rh D negative population both in the test and control groups respectively. This pattern of result was observed in a similar study by Ukaejiofo and Nubila, [32] who found no association between ABO blood group and HIV infection. Also a similar study by Igbenegbu et al. [33] corroborated this finding that the ABO blood group system does not seem to have an influence on HIV infection [33].
The blood group and haemoglobin genotype of an individual has been observed to have little to do with occurrence of disease as do finger print, colour of hair or eyes [34], this study support this findings with the haemoglobin types in both the patient and control groups distributed in the same general pattern (Hb AA, AS and AC) notwithstanding the HIV status of the test group.
The role of CD4 has a major predictor of disease progression and monitoring of the effectiveness of highly active antiretroviral therapy (HAART) in HIV infection along with the HIV-RNA level cannot be overemphasized in HIV infection. CD4+ cells counts are influenced by genetic, immunological, physiological, and behavioral factors exhibited by an individual [34-35], and they vary widely both within and among populations. Expectedly, this study reveals that the mean CD4 cell count in HIV infection is lower than that of control with a significant association p<0.05, which further validate the immune suppressive role of the HIV on the T cells (Table 1).
Surprisingly, the CD4 cell distributions in the different blood groups differ between the subject and control groups. Findings from this study reveal that blood group A patients have the predominant CD4 cell count while the control group had CD4 count highest in blood group O, followed by groups A, B and AB (Fig. 1). This finding implies that blood group A confers a form of resistance to immunosuppression in such patients and this is indeed established by the increased CD4 cell level also observed in blood group AB before other groups. A study by Ayatollahi et. al. [36] also reveals that there is an association between A Rh D positive Human T-lymphotropic (HTLV) viruses infected individual and healthy controls and the results suggested that the A+ blood group decrease the risk of HTLV-1 infection in healthy controls, while the AB+ blood group is more frequent in HTLV-1 carriers and increases the risk of HTLV-1 infection [36]. In addition findings from a similar study conducted by Arendrup et. al. [37], which was also substantiated by Neil and colleagues in a similar study [38], reported that HIV from lymphocytes of blood group A individuals was neutralized by anti-A, implying that this mechanism could potentially reduce the likelihood of infection in ABO discordant couples [38].
CONCLUSIONS
This study validate previous studies that ABO/Rh antigens and Haemoglobin electrophoretic patterns are not associated with HIV infection but CD4 T- cells level is significantly associated with ABO blood groups in HIV infection with blood group A and AB having increased CD4 cell count thereby contributing to increased immune resistance in such individuals. There is therefore need to determine the mechanism and substances responsible for this immune protective action.
REFERENCES
| International Journal of Life-Sciences Scientific Research (IJLSSR)
Open Access Policy
Authors/Contributors are responsible for originality, contents, correct
references, and ethical issues.
IJLSSR publishes all articles under Creative Commons
Attribution- Non-Commercial 4.0 International License (CC BY-NC). https://creativecommons.org/licenses/by-nc/4.0/legalcode |
| How to cite this article: Bamisaye EO, Adepeju AA, Akanni EO, Akinbo DB, Omisore AO: Association between Blood Group Antigens, CD4 Cell Count and Haemoglobin Electrophoretic Pattern in HIV Infection. Int. J. Life. Sci. Scienti. Res., 2017; 3(5):1300-1304. DOI:10.21276/ijlssr.2017.3.5.6 Source of Financial Support:Nil, Conflict of interest: Nil |